Abbott
CentriMag Circulatory Support Systems Clinical Reference Manual Rev 00
Clinical Reference Guide
32 Pages
Preview
Page 1
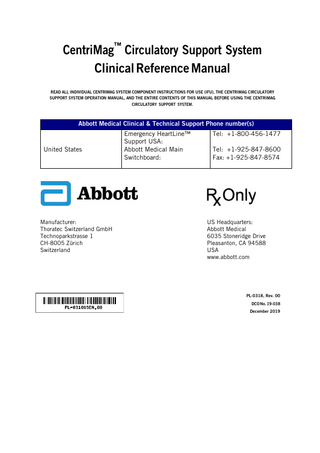
CentriMag™ Circulatory Support System Clinical Reference Manual READ ALL INDIVIDUAL CENTRIMAG SYSTEM COMPONENT INSTRUCTIONS FOR USE (IFU), THE CENTRIMAG CIRCULATORY SUPPORT SYSTEM OPERATION MANUAL, AND THE ENTIRE CONTENTS OF THIS MANUAL BEFORE USING THE CENTRIMAG CIRCULATORY SUPPORT SYSTEM.
Abbott Medical Clinical & Technical Support Phone number(s)
United States
Manufacturer: Thoratec Switzerland GmbH Technoparkstrasse 1 CH-8005 Zürich Switzerland
Emergency HeartLine™ Support USA: Abbott Medical Main Switchboard:
Tel: +1-800-456-1477 Tel: +1-925-847-8600 Fax: +1-925-847-8574
US Headquarters: Abbott Medical 6035 Stoneridge Drive Pleasanton, CA 94588 USA www.abbott.com
PL-0318, Rev. 00 DCO No. 19-038 December 2019
™ Indicates a trademark of the Abbott group of companies. ‡ Indicates a third party trademark, which is property of its respective owner. Pat. http://www.abbott.com/patents © 2019 Abbott. All Rights Reserved.
3
Contents Introduction ... 6 Indications for Use ... 6 Contraindications ... 6 Potential Adverse Events ... 6 Warnings and Cautions... 6 Terminology and Abbreviations ... 7 Description ... 7 Clinical Use of the CentriMag Circulatory Support System ... 8 General Principles ... 8 Types of Support ... 9
Preparing for CentriMag System Use ... 9 System Setup... 9 Alternatives for Pump Priming and De-airing ... 9 Priming Pack Technique ... 9 Submersion Priming Technique ... 10 Cannulas ... 12
Surgical Technique for Implantation ... 13 Overview ... 13 Monitoring ... 13 Tunneling... 13 Cannula Site Selection and Cannulation ... 14
Intraoperative Device Management ... 15 Guidelines to Prevent Air Entrainment when Initiating Support ... 15
Patient Care and Management... 15 Guidelines to Prevent Air Entrainment during Support ... 16 CentriMag System Assessment and Adjustments ... 16 Hemodynamic Assessment and Support ... 17 Intra-aortic Balloon Pump ... 17 Defibrillation/ Cardioversion... 17 Anticoagulation ... 18 Wound Care ... 18 Nutrition ... 18 Physical Therapy ... 18 Patient Transport ... 18 Prevention and Management of Potential Complications... 19 Alarms/Alerts and Troubleshooting ... 20
Weaning and Explantation ... 20 Weaning Protocol ... 20 Pump Exchange ... 21 Explantation ... 21
Summary of Clinical Experience... 21 Study Design ... 22 Accountability of the FTW Study Cohorts ... 24 Study Population Demographics and Baseline Parameters ... 25
4
Safety and Effectiveness and Results ... 27 Device Malfunctions and Failures ... 30 Clinical Study Safety and Effectiveness Conclusions ... 33
5
Introduction This manual is designed for healthcare professionals. It contains clinical and technical information for guidance in the proper and safe use of the CentriMagTM Circulatory Support System when used as intended. The information in this manual supplements the CentriMag Circulatory Support System Operation Manual and each of the individual system component instructions for use. The CentriMag system performs life-sustaining functions. Users should have a practical knowledge of the principles of mechanical circulatory support and should be aware of the physiological and psychological needs of a patient undergoing mechanical circulatory support. New users should read this manual in its entirety before system operation. For experienced practitioners, this manual may serve as a reference. As with all prescription medical devices, clinical procedures should be conducted under the direction of the prescribing physician. The professional staff at Abbott Medical regularly provide laboratory training and on-site, in-service programs. For information, please contact your local Abbott Medical Clinical Field representative.
Indications for Use The Indications for Use for the CentriMag Circulatory Support System include the following: The CentriMag Circulatory Support System is indicated for use as part of a cardiopulmonary or other extracorporeal bypass circuit for periods up to 6 hours [510k-cleared Device]. The CentriMag Circulatory Support System is indicated for temporary circulatory support for up to 30 days for one or both sides of the heart to treat post-cardiotomy patients who fail to wean from cardiopulmonary bypass, providing a bridge to decision when it is unclear whether the patient's heart will recover or whether the patient will need alternative, longer-term therapy [PMA Approved Device]. The CentriMag Circulatory Support System is indicated for use as a right ventricular assist device [Humanitarian Device]. The system, when used as a right ventricular assist device, is also authorized by Federal law to provide temporary circulatory support for up to 30 days for patients in cardiogenic shock due to acute right ventricular failure. The effectiveness of this device for this use has not been demonstrated.
Contraindications The CentriMag Circulatory Support System is contraindicated for use as a cardiotomy suction device. The system is also contraindicated for patients who are unable or unwilling to be treated with an appropriate anticoagulant such as Heparin or a comparable alternative.
Potential Adverse Events Adverse events (e.g., complications) are a known risk of mechanical circulatory support use. The adverse events observed during four clinical studies of the CentriMag system are listed below. The adverse events are listed in decreasing order of frequency, except for death, because it is a non-reversible complication. There were no unexpected adverse events observed in these studies. For the incidence summary of all the adverse events that were observed, refer to the Summary of Clinical Experience section.
Death Bleeding Respiratory Failure Infection Cardiac Arrhythmias Renal Failure/Dysfunction Right Heart Failure Neurologic Dysfunction Hemolysis Hepatic Dysfunction Hypotension Venous Thromboembolism Hypertension Cardiac Tamponade Psychiatric Episode Pericardial Fluid Collection Device Malfunction Wound Dehiscence Arterial Non-CNS Thromboembolism Limb Ischemia Myocardial Infarction Aneurysm
Warnings and Cautions Warnings are used if there is a potential for a serious hazard with misuse of the device, when special attention is required for safety of the patient, or when special care should be exercised to prevent improper operation of the device that may cause damage. Cautions are used to alert the user to exercise special care for the safe and effective use of the device.
6
Terminology and Abbreviations Abbreviations for terms used in this manual include: ABP, arterial blood pressure ACT, activated coagulation time AMI, acute myocardial infarction BiVAD, biventricular assist device BUN, Blood Urea Nitrogen CI, cardiac index CPB, cardiopulmonary bypass CVP, central venous pressure ECMO, extracorporeal membrane oxygenation FTW, Failure to wean HIT, Heparin-induced thrombocytopenia IABP, intra-aortic balloon pump IJ, internal jugular LAP, left atrial pressure LPM, liters per minute LVAD, left ventricular assist device MAP, mean arterial pressure mmHG, millimeters of Mercury PADP, pulmonary artery diastolic pressure PCCS, Post-cardiotomy cardiogenic shock PCWP, pulmonary capillary wedge pressure PFO, patent foramen ovale PTT, partial thromboplastin time PVR, pulmonary vascular resistance
RAP, right atrial pressure RPM, revolutions per minute RVAD, right ventricular assist device TEE, transesophageal echocardiography TEG, thromboelastography
Description The CentriMag system is designed to provide a versatile and effective means for implementing mechanical circulatory support in a variety of clinical scenarios. The system is intended to treat acute heart failure by decreasing ventricular workload, stabilizing hemodynamic conditions, and facilitating potential myocardial recovery. Patients in acute cardiac failure are at risk of developing multisystem organ failure which can threaten long-term survival. For these patients, the CentriMag system can provide short-term circulatory support pending recovery of ventricular function or provide a means to hemodynamically stabilize the patient until an alternative, longer-term therapy can be implemented. The core components of the system include a CentriMag Blood Pump, 2nd Generation CentriMag Primary Console, motor, Mag Monitor, flow probe, tubing, and cannulas. Figure 1. CentriMag system 1. Cart 2. Monitor 3. Pump 4. Motor 5. Console 6. Backup motor 7. Backup console
7
The primary design features of the system include:
Fully magnetically levitated impeller No bearings, shafts, valves, or seals within pump Low priming volume (31 cc) designed to reduce hemodilution Disposable (polycarbonate) pump with standard 3/8” connectors Reusable motor, console, non-invasive flow probe and accessories Configurable as an LVAD, RVAD, or BiVAD
The CentriMag pump is a continuous flow, fully magnetically levitated centrifugal pump. When the pump is inserted into the motor and activated, the internal impeller is electromagnetically levitated and centered. Large gaps between the impeller and pump housing are designed to minimize potential shear forces on blood cells, allowing a high blood flow rate with minimal hemolysis and thrombosis. Full MagLevTM technology suspends and rotates the impeller without a physical bearing. The pump contains an inflow port on the top and an outflow port on the side that are at right angles to one another, as well as a magnetically levitated impeller. When the impeller is rotated, a pressure gradient develops between the center and outside edge of the pump, causing blood to flow from the inflow to the outflow port of the pump. The rotation of the impeller, as well as the resulting blood flow, is not sensitive to the pump height or position. The amount of flow through the pump depends on the set speed of the impeller, and the difference between the inlet and outlet pressures. Factors affecting the flow include the following:
Pump speed
Preload pressure
Afterload pressure Inflow cannula size, resistance and position Outflow cannula size, resistance and position Tubing length
Figure 2. CentriMag pump 1. Inflow port 2. Impeller 3. Outflow port
Flow is generated by the rotation of the pump impeller. The blood flow is measured by a clamp-on, non-invasive flow probe and displayed on the console screen and optional monitor. The speed of the pump must be set high enough to overcome native cardiac pressure in order to prevent retrograde flow. Increasing the RPM will increase the flow of blood through the pump. CAUTION: If an increase in set speed does not cause an increase in flow, lower the set speed and assess the position of the cannula and the patient's hemodynamic condition. During patient support, the console is used to control pump speed, the resultant blood flow, and to monitor the safe operation of the system. A cable connects the console to the motor, allowing flexibility in the pump motor and pump positioning. When needed, a battery in the console will power the system for two hours. An additional console and motor should be available at all times for emergency backup. For system specifications, refer to the CentriMag Circulatory Support System Operation Manual.
Clinical Use of the CentriMag Circulatory Support System General Principles The CentriMag system provides circulatory assistance for patients in acute hemodynamic compromise, a population whose treatments options are limited. WARNING: Read this entire manual before you use the CentriMag System. As with all prescription medical devices, clinical procedures should be conducted under the direction of the prescribing physician. The physician must be trained on the use of the System before using it. The professional staff at Abbott Medical regularly provide laboratory training and on-site, in-service programs. For information, please contact your local Abbott Medical Clinical Field representative. Temporary circulatory support with the system can restore hemodynamic stability, reduce the risk of further end-organ damage, and provide conditions under which organ function can recover. By stabilizing the hemodynamics and optimizing the patient’s condition, the patient's end-organ function can be assessed to determine the clinical course for the patient. In many cases, myocardial and end-organ recovery will be sufficient to allow weaning the patient from CentriMag system support. Some patients may need long-term support with an implantable LVAD or a heart transplant.
8
WARNING: The safety and effectiveness of use of the CentriMag system in an ECMO circuit (i.e. cardiopulmonary support > 6 hours) has not been demonstrated. WARNING: The safety and effectiveness of use of the CentriMag system for use > 30 days has not been demonstrated. Patients undergoing cardiac surgery who fail to be weaned from cardiopulmonary bypass due to poor cardiac function or high risk of dysrhythmias may benefit from continued circulatory support with a ventricular assist device. In this post-cardiotomy scenario, CentriMag system support can be initiated quickly without significant additional resources. Patients can then be transferred to a recovery area or intensive care unit in a hemodynamically stable condition. Further patient assessment and treatment options can then be considered.
Types of Support The CentriMag system can be used as an LVAD, RVAD, or BiVAD as described in the sections below.
Isolated LVAD Support When compromised or impaired left ventricular function results in a patient being unable to wean from cardiopulmonary bypass, CentriMag LVAD support may be beneficial. Cannulation options include placement of a drainage cannula in the left atrium or left ventricle with a return cannula placed or attached to the ascending aorta, axillary artery, or a femoral artery.
Isolated RVAD Support Patients who may require isolated RVAD support include those in cardiogenic shock due to acute right ventricular failure 1 or those whose right ventricular function is too compromised to wean from cardiopulmonary bypass. Patient history and pre-implant assessment of the heart using cardiac echocardiography and a determination of PVR should help to identify patients who will benefit from RVAD support for cardiogenic shock. Cannulation options are placement of a drainage cannula in the right atrium, right ventricle, superior vena cava, or inferior vena cava, with a return cannula in the pulmonary artery.
RVAD Support following LVAD Implantation 2 RVAD support may be required following implantation of a durable LVAD. Initiating LVAD support can cause an acute decrease in left ventricular pressure that can change the position of the intra-ventricular septum, lead to distention of the right ventricle, and an increase in right atrial pressure. Under these conditions, right atrial pressures above 15-20 mmHg are suggestive of right ventricular dysfunction. Such a condition is often associated with a decrease in right ventricular contractility and tricuspid insufficiency. If adequate LVAD flow cannot be achieved, and there are signs of right heart failure, it may be necessary to temporarily support the right ventricle with a CentriMagTM RVAD. Diagnostic assessments include cardiac echocardiography, measurement of right heart pressures, and if possible, direct visualization of right ventricular function.
Biventricular Support Biventricular support may be necessary in instances where the entire heart is functioning too poorly to wean a patient from cardiopulmonary bypass.
Preparing for CentriMag System Use The CentriMag system components and supplies are often stored in the operating room area to be immediately available when needed. The consoles must be connected to AC power during storage to ensure that the batteries are always fully charged. A backup system must always be close to the patient in the event it becomes necessary to switch to backup system components.
System Setup System setup and initiation of support is often performed under emergent conditions. The procedure for setting up the CentriMag system, as described in the CentriMag Circulatory Support System Operation Manual, may be tailored to meet the anatomical and clinical conditions of individual patients. Different methods for priming the pump and circuit are discussed below. After the setup and priming steps are completed, all of the connections should be secured with bands. CAUTION: Ensure that the tubing is secured with bands on a portion of the connection where the two components overlap ( i.e. where the tubing covers the pump inlet). The tubing should be over the lip of the pump connector.
Alternatives for Pump Priming and De-airing Priming should be performed using either a priming pack or circuit submersion technique that follows standard surgical protocols. Two alternatives are described below.
Priming Pack Technique Typical Contents The following is a suggested list of equipment and supplies that may be used with a pre-assembled circuit or priming pack. 3 1 2 3
Humanitarian Use. The effectiveness of this device for this use has not been demonstrated. Humanitarian Use. The effectiveness of this device for this use has not been demonstrated. For the pumps, you will need one for univentricular support, two for biventricular support, plus a backup. For the console with motor and flow probe connected, you will need one of
9
CentriMagTM pumps Drainage cannulas Return cannulas 2nd Generation CentriMagTM console with motor and flow probe connected Preassembled circuit and priming pack Two 3/8” two-sided, straight, barbed connectors (and backups), if not included with the cannula kits Sterile tubing clamps and scissors One liter of a warm balanced electrolyte solution for priming Small nylon bands (~3” in length)
Typical Priming Pack Procedure The priming pack procedure should be performed using aseptic techniques. To prime the pump: 1.
Open the priming pack. Open the pump package. Attach the drainage tubing and return tubing to the appropriate barbed ports of the pump. Suspend the recirculation bag from an IV pole. CAUTION: The outside of pump packaging is not sterile.
2.
When possible, flush the recirculation bag and circuit with CO2 to remove air. Clamp the outlet lines from the reservoir bag. Fill the reservoir bag with one liter of a balanced electrolyte solution. Open the reservoir bag air vent line. CAUTION: Maintain an adequate level of priming solution in your reservoir bag at all times to prevent depriming the circuit.
3.
Raise the pump up to the level of the bag. Remove the clamps from the reservoir bag outlet lines. Slowly fill the circuit with fluid by “walking” the fluid through the circuit, while venting the air through the vent line. CAUTION: When the clamps are removed, ensure that you are priming the tubing slowly to minimize the risk of air entrainment.
4.
Secure and lock the pump in the motor mount and recirculate the fluid at a low flow of approximately 1500 RPMs. CAUTION: Ensure that the pump is properly seated, aligned, and locked into the motor.
Submersion Priming Technique Typical Contents The following is a suggested list of equipment and supplies that may be used for this technique. 4
CentriMag pumps Drainage cannulas Return cannulas 2nd Generation CentriMag console with motor and flow probe connected Standard 3/8”ID x 3/32” wall tubing Two 3/8” straight barbed connectors per pump, if not included with the cannula kits Sterile tubing clamps and scissors Three liters of warm balanced electrolyte solution Bulb syringe and scissors Small nylon bands (~ 3” in length)
Submersion Technique – Dry Connection The dry connection submersion technique should be performed using aseptic techniques. To prime the pump: 1.
Fill a large sterile basin with three liters of a warm balanced electrolyte solution.
2.
Open the pump package. Connect the inlet and outlet of the pump to separate segments of the tubing. CAUTION: The outside of pump packaging is not sterile.
3.
Slowly submerge the open side of the drainage tubing segment, then gradually submerge the entire piece, allowing the tubing to fill completely from one end to the other, remaining under the surface at all times. Allow the pump to fill and deair. Continue filling past the pump until the return tubing segment is also filled and deaired. CAUTION: Avoid striking the pump housing in order to force air through the circuit, as damage to the pump housing may occur.
4.
Once the circuit is completely primed and deaired, clamp both open ends of the tubing.
5.
Pass the pump off the field (leave the ends of the tubing in the basin and maintain sterility of the tubing above the area which was passed off) and place the pump in the motor.
6.
Connect the flow probe to the return segment of the tubing.
each for univentricular support, two of each for biventricular support, plus one of each for backup. 4 For the pumps, you will need two pumps for univentricular support and three pumps for biventricular support. For the console with motor and flow probe connected, you will need one of each for univentricular support and two of each for biventricular support.
10
7.
Turn on the console, and set the speed to approximately 1500 RPMs with the clamps still on the drainage and return tubing in the basin.
8.
Remove the clamp from the drainage tubing and then remove the clamps from the return tubing. Allow the priming solution to recirculate until all visible air is removed. CAUTION: Ensure that the open ends of the tubing segments remain submerged during recirculation to avoid air entrainment.
9.
Inspect the circuit to ensure all air has been removed. If there is residual air, continue to run the pump with the open ends of the tubing in the basin to complete the de-airing process. CAUTION: If air is entrained in the pump head, turn the set speed to zero, and then walk the air bubble out of the pump.
10.
Replace the clamps on the inflow and outflow tubing in the basin. The circuit is now ready for use.
Submersion Technique – Wet connection The wet connection submersion technique should be performed using aseptic techniques. To prime the pump: 1.
Fill a large sterile basin with three liters of a warm balanced electrolyte solution.
2.
Slowly submerge one end of the drainage tubing segment, then gradually submerge the entire piece, allowing the tubing to fill completely from one end to the other, remaining under the surface at all times. Clamp both ends of the tubing segment once all air has been dispelled and tubing is primed. Repeat for the return tubing segment. CAUTION: The CentriMag pump may magnetically attract to a metal basin. Use caution if a metal basin is used.
3.
Open the pump package. Submerge the pump in the saline, rotating from side to side to ensure complete removal of air. CAUTION: The outside of the pump packaging is not sterile.
4.
Remove the clamp from one end of the drainage tubing segment and then connect it to the inflow of the pump. Remove the clamp from one end of the return tubing segment and then connect it to the outflow of the pump. Ensure that all of the connections are made while the components are fully submerged.
Figure 3. Submersion of tubing
11
Figure 4. Submersion of pump
Cannulas For left and/or right sided support for failure to wean, Abbott Medical recommends the CentriMagTM Drainage (Venous) Cannula (34Fr) and Return (Arterial) Cannula (24Fr). Other equivalent commercially available venous and arterial cannula may be used at the preference of the clinician. For central cannulation, it is advisable to use cannulas that are wire-reinforced to resist kinking. The drainage cannula should be malleable so that it will hold its shape after introducing a bend. For ventricular cannulation, the drainage cannula may not need to be bent. Placing an approximately 90º bend in the cannula may help with atrial cannulation.
12
Surgical Technique for Implantation Overview This section describes the surgical considerations necessary to prepare, implant, and explant the CentriMag system. Standard surgical techniques will be used for implantation of the system. The components of the circuit will be similar for most patients, although the surgical procedures may vary according to the patient’s anatomy, circumstances of support initiation and hospital protocols. In general, the procedures are as follows: the cannulas are tunneled and positioned for left, right, or biventricular support. The extracorpeal circuit (or circuits) is prepared, primed, connected to the cannulas, and subjected to a final inspection of the circuit; support is then initiated. If CentriMag cannulas or other centrally-placed cannulas are used, the surgical approach for implantation will usually include the following general order of process: 1.
Sternotomy
2.
Tunneling
3.
Cannulation
If the condition and stability of the patient permit, all cannulas should be tunneled and brought through the skin of the anterior abdominal wall (the subcostal region) prior to cannulation of the heart and major vessels. For left heart LVAD support, the drainage cannula will be placed in the apex of the left ventricle or left atrium and the return cannula will usually be placed in the ascending aorta. If ambulation is planned, consideration should be given to placement in the axillary artery. If an RVAD for right heart support is needed, the drainage cannula will usually be placed in the right atrium and the return cannula will be placed in the proximal portion of the main pulmonary artery. CAUTION: The position of the drainage cannula in the left ventricular apex should be positioned pointing toward the mitral valve (the tip should be placed in the direction of the mitral valve) in order to maximize drainage and minimize suction events. CAUTION: The preferred placement of the return cannula is in the ascending aorta. Confirm that the point of anastomosis is not calcified to avoid the risk of a stroke. The circuit is primed with a balanced electrolyte solution, deaired, and inspected. Connection of the primed circuit to the cannula connector is made while adding fluid to the connection to exclude air. The cannulas are secured to the skin with sutures. All external connections should be further secured with bands for added security and circuit integrity. The pump is positioned on the motor and the console is powered on and speed set to at least 1000 RPMs with a clamp on the outlet tubing. CAUTION: If the clamps are removed before the speed is set higher than 1000 RPMs, there is a risk of retrograde flow. NOTE: If other manufacturers’ cannulas are used, follow standard surgical techniques applicable to those cannulas. The status of the heart is monitored with echocardiography, hemodynamic monitoring, palpation, and direct visualization, to ensure adequate intravascular volume, CPB flow is reduced while VAD support is initiated. After cannulation, the sternum and skin are closed using standard surgical techniques. If unable to close the sternum due to mediastinal bleeding, or if edema causes compromised flow, the chest may be packed, sternum splinted open, and the skin opening covered with an appropriate patch for closure later.
Monitoring Hemodynamic assessment before and during CentriMag system support should include standard cardiac surgery pressure monitoring such as a central venous catheter, an arterial line, and a pulmonary artery catheter. Before initiating CPB and placement of the CentriMagTM cannulas, transesophageal echocardiogram should be performed to rule out the following:
A patent foramen ovale or other septal defects Intra-atrial and intra-ventricular thrombus Aortic valve insufficiency Valvular dysfunction Any other structural abnormalities that may interfere with the safe operation of the device (i.e. trabeculae or ruptured chordae)
TEE should be used to visualize the heart chambers and to ensure that the heart is completely deaired prior to initiation of support. TEE may also be used to assess cannula tip position, ventricular volume, ventricular size, optimal neutral position of the ventricular septum, and the amount of unloading in the heart chambers. If CPB is used for the implant, anticoagulation appropriate for CPB must be administered before CPB. If the implant is to be performed without CPB, heparin should be administered to the patient prior to cannulation with a recommended target of an activated coagulation time between 200 and 250 seconds.
Tunneling The cannulas should be tunneled through the chest wall using a standard surgical technique. It is recommended that tunneling be performed prior to cannulation so that the cannula can be positioned without bends or kinks. Prior to tunneling, cover the tip of the cannula with the included tunneling cap, or if none is included, a glove tip or other material to prevent debris from entering the internal lumen. At the end of the case, the cannulas should be securely sutured to both fascia and skin, with minimal tension. For more information, refer to the instructions for use for the cannulas. CAUTION: If the cannula kit does not include a tunneling cap, use caution to not tear or damage the glove tip or other material to prevent damaging the cannula connector.
13
Cannula Site Selection and Cannulation Common cannulation 5 locations are shown in the table below. Table 3. Cannulation locations Therapy LVAD support
Access Point Central
Drainage Vessels Left Atrium Left Ventricle
Return Vessels Ascending Aorta Via direct cannulation or with a graft sewn to ascending aorta Axillary Artery
RVAD support
Central Peripheral
Right Atrium Right Ventricle Superior Vena Cava Inferior Vena Cava
Pulmonary Artery Via direct cannulation or with a graft sewn to pulmonary artery
BiVAD support
Central Peripheral
See options above for left and right sided support
See options above for left and right sided support
Two cannulation approaches are shown in the figures below. The left ventricle is drained via the left ventricular apex or the left atrium. In both approaches, blood is returned via the ascending aorta. Left ventricular cannulation may be preferred because the unloading is more complete, the risk of intra-ventricular thrombus is much lower, and collapse of the chamber is less likely, though care should be taken to minimize the risk of suction. Figure 5. Drainage via the left ventricular apex
Figure 6. Drainage via the left atrium
5 The CentriMag Return (Arterial) Cannula and the CentriMag Drainage (Venous) Cannula are not intended for peripheral cannulation.
14
Intraoperative Device Management After all cannula-to-tubing connections are completed, a clamp is placed on the return tubing of each pump, while all other clamps are removed from the circuit. Before the outflow clamp is released, the pump set speed (RPM) is increased to at least 1,000 RPM in order to prevent retrograde flow through the system. The set speed is then gradually increased to reach the desired flow rate. As the set speed is gradually increased, CPB support can be simultaneously decreased to allow filling of the heart, and then terminated. During weaning from CPB and initiation of CentriMag system support, the patient must be carefully monitored with hemodynamic monitoring (usually CVP, PAP and ABP), echocardiography, manual palpation and visual inspection of the heart to ensure that adequate blood volume is available for the desired flow and to reduce the risk of a suction event. For LVAD support, left atrial pressure should be maintained between 10 and 15 mmHg in order to avoid suction within the left ventricle and inflow obstruction, which can lead to air entrainment. For RVAD support, right atrial pressure should also be maintained between 10 and 15 mmHg. CAUTION: Ensure that air does not enter into the circuit when the tubing is connected to the cannula. CAUTION: If CPB support is not decreased as the set speed is increased, suction events may occur due to lack of volume. The desired flow rate can be predetermined by calculating the flow needed to achieve a cardiac index of approximately 2.0-2.2 l/min/m2. As the flow is increased, the atria and/or ventricles are monitored for adequate pressure and blood volume. The console operator continuously monitors the pump flow, RPM, and blood pressure for signs of suction within the circuit. Suction is most likely when filling pressures are <10 mmHg and is accompanied by fluctuations in flow. When suction is detected, the speed of the pump must be immediately decreased until the filling pressure and volume are adequate to increase the flow. The system should be monitored frequently in the operating room when the patient’s chest is open as this is the period of highest risk for suction and air entrainment. The central venous pressure, flow rate, total cardiac output, pulmonary capillary wedge pressure, left atrial pressure (valuable, but not essential) and arterial blood pressure should be monitored frequently as hemodynamic conditions change rapidly during surgery. Communication of hemodynamic parameters between the surgeon, perfusionist, anesthesiologist, and console operator is vital to safe support. Initially, TEE, hemodynamic monitoring, palpation, and direct visualization of the heart will help to determine the volume of blood available for the circuit and the optimal level of flow. After the chest is closed, the patient can be monitored with conventional hemodynamic parameters (CVP, PCWP, MAP, LAP, PADP) and TEE to ensure adequate ventricular unloading, and to permit a gradual increase to a target CI between 2.0 and 2.5 l/min/m2, consistent with the patient’s physiologic needs. CAUTION: After closure of the chest, limited space in the inter-thoracic cavity may cause an observable decrease in flow. TEE should also be used to rule out the presence of a patent foramen ovale after left ventricular decompression. A previously undetected PFO may develop when the pump begins to decompress the left heart. If present, a significant defect should be repaired to prevent right-to-left shunting and the resulting hypoxemia. Unloading of the ventricle(s) during VAD support may also cause atrial or ventricular collapse, which may be able to be observed or assessed with manual palpation by the surgeon. CAUTION: During closure of the chest, the CentriMag system flow and the patient’s hemodynamics must be monitored as cannula position can change, altering flow through the pump.
Guidelines to Prevent Air Entrainment when Initiating Support Guidelines to prevent air entrainment when initiating support include the following: 1.
Fill the chest with warm normal saline or CO2.
2.
Ensure adequate volume in heart chamber when coming off CPB bypass.
3.
Watch the circuit, flow, CVP, MAP and LAP (if monitored) continuously and be prepared to immediately clamp the outflow tubing if air is observed.
4.
Partially inflate the lungs prior to separation from CPB.
5.
Maintain atrial pressures between 10 and 15 mmHg during surgery.
6.
Place the patient in Trendelenburg position.
7.
Check the heart and aorta for air with TEE.
8.
Increase RPM very slowly while initiating support.
9.
Under-perfuse circulation while the chest is open or patient is being moved. CAUTION: If an increase in flow is not observed with an increase in set speed, suction may be occurring. WARNING: If a suction event occurs and is not addressed promptly, there is potential for air entrainment.
Patient Care and Management Postoperative care with the CentriMag system is similar to other types of mechanical circulatory support. Key principles of care include hemodynamic stabilization, adequate anticoagulation, and prevention of wound infection. The intravascular volume must be carefully assessed and controlled. Management of bleeding, and prompt blood product replacement, is essential to stabilization and recovery. Frequent laboratory assessment of hematology, coagulation, enzymes, and blood chemistry must be used to evaluate end organ function and to guide therapy.
15
Guidelines to Prevent Air Entrainment during Support Guidelines to prevent air entrainment during support include the following:
Monitor the volume with TEE and pressures. Reduce CentriMag flow rate while the chest is open. Reduce RPM for any indication of inadequate volume, during manipulation of the heart, or prior to moving the patient. Monitor the tubing for chatter and be prepared to respond by decreasing RPMs and giving volume. As soon as practical, set the low-flow alarm at 75% of the target flow. Train staff that air can be drawn into the vasculature by the flow characteristics of circulatory support: Through any open stopcock or port on central line Through an IV or infusion line During insertion/changing of a central line with an open port. Be sure there are no signs of suction during insertion of a central line. Through any loose connection point on the system circuit Avoid conditions that may result in suction, line chatter, or shaking.
CentriMag System Assessment and Adjustments Pump speed and alarm settings must be assessed frequently and manually adjusted when necessary. Speed changes should be gradual while monitoring the changes in available volume and the resultant hemodynamic effects. Ensure that you clamp the return tubing prior to turning off the pump or reducing set speed below 1000 RPM to avoid retrograde flow. Pump flow (LPM) and speed (RPM) should be recorded with vital signs on the patient’s chart to trend hemodynamic change with the pump parameters. Table 4. Target pump and clinical conditions Parameter
6
CentriMag pump
Value 3000-4000 RPM
Pump flow
4-5 LPM
RAP and LAP
10-15 mmHg [8-12 mmHg after several stable days of support]
Mean arterial pressure
60-80 mmHg
Target ACT
160-180 seconds (after bleeding has subsided)
For biventricular support, the hemodynamic conditions of the pulmonary and systemic circulations should be balanced. To do this, manage the RVAD flow relative to the LVAD flow. Increase or decrease the RVAD set speed gradually, in 50-100 RPM increments every few seconds, allowing the patient’s vascular system to adjust between each RPM change. The pump set speed should be gradually increased to the desired flow. If flow drops or tubing chatter is observed, the set speed should be immediately reduced 100-200 RPM. Once target flows are acquired, if changes are necessary to one of either the LVAD or RVAD flows, ensure that the other is also changed accordingly. CAUTION: If the RVAD speed is increased but no change in the LVAD flow is observed, a pulmonary edema may be present. Decrease the RVAD set speed, and increase the LVAD set speed as needed to balance appropriately. CAUTION: If the LVAD speed is increased without adjusting the RVAD speed, risk of LV suction may occur. Normally the left heart output is slightly greater than the right heart due to natural shunting. When providing maximal support, the right and left pump flows should be nearly equal, but may vary as much as 0.5 LPM to 1.0 LPM, with the left side support usually being greater. The factors that affect this difference are the valvular incompetence, and ventricular ejection through the pulmonic or aortic valves, that is not reflected in the VAD flow. Generally, the right flow should not greatly exceed the left flow. WARNING: A high RVAD pulmonary flow without a corresponding high LVAD systemic flow may result in pulmonary edema. The position of the flow probe should be such that it does not cause kinking of the tubing. If positioned close to the pump, the weight of the flow probe may cause a kink in the tubing near the inlet or outlet of the pump. Moving the probe further away from the pump will usually resolve this. Repositioning the flow probe on the tubing line periodically to maintain accuracy and avoid kinking of tubing is recommended. Periodic checks should be performed to ensure:
There is no entrained air. There are no clots at tubing connections to the cannulas and pump. A flashlight can be used to inspect. Cannulas are secured to the patient. Tubing is free of sharp bends or kinks. The console is on AC power. The battery is fully charged. An additional console is available to use as a backup console.
6 Actual patient values will vary significantly based on individual needs and hemodynamic condition.
16
The low flow alarm is set. This should be set at approximately 75% of the desired clinical flow. There is air circulation around the motor and console. There are two tubing clamps near each pump.
Staff should periodically rehearse switching to the backup motor and console using a spare system and training (mock circulatory) loop. Refer to the CentriMag Circulatory Support System Operation Manual for details.
Hemodynamic Assessment and Support Hemodynamic monitoring during support with the CentriMag system has some special considerations. During LVAD support, the arterial pressure waveform will normally show a significantly reduced pulse pressure (Systolic-Diastolic) when the left ventricle is completely unloaded. An increase in the pulse pressure will be observed as the ventricle recovers, when the pump flow is decreased, or if the volume status of the patient is increased. A similar change will be seen on the pulmonary artery waveform during RVAD support. Pulmonary artery catheters may prove useful for monitoring during CentriMag system support, but there are some important considerations during RVAD support. First, because the pulmonary artery catheter is inserted and maintained in position with the aid of blood flow through the right heart, insertion of a catheter during RVAD support is usually not possible. Pulmonary artery catheters that are in place before RVAD implant may be used for pressure monitoring and mixed venous oxygen saturation only, but often can migrate out of the pulmonary artery. Thermodilution or continuous cardiac output determinations are inaccurate during RVAD support. Since the inflow and outflow cannulas are placed in the right atrium and pulmonary artery, the majority of the circulating blood travels through the pump circuit, rendering the pulmonary artery flow measured by the catheter incorrect. The RVAD flow bypasses the thermistors that measure the temperature changes needed for the cardiac output measurement. However, in most cases the mixed venous oxygen saturation may be used to estimate changes in total cardiac output based on the Fick principle. CAUTION: The usual thermodilution methods for measuring total cardiac output might be inaccurate, and pump flow may not represent total cardiac output. Although the CentriMag system may capture the majority of blood flow, some ventricular output may be through the aortic or pulmonic valve. CentriMag system flow may also be elevated due to shunts or incompetent valves. Adequate volume is essential for pump operation. Fluid balance should be routinely monitored using patient weight, CVP, LAP, and/or PCWP, with careful attention to intake and output. If there is significant diuresis, intravascular fluid shifts or bleeding, this will adversely affect the available blood volume needed to operate the system, and the flow may need to be temporarily reduced while these conditions are treated. If a CVP catheter needs to be placed during CentriMag system support, care must be taken to avoid air entrainment during placement. Consider temporarily decreasing the RPMs during insertion. This will make it easier to see the IJ or subclavian. Place the patient in the Trendelenberg position, if tolerated. Be sure there are no signs of negative pressure during insertion (line chatter, ramping of the flows, or flow below the minimum alert). Place a stopcock on the open ports of the central line to avoid air being entrained. CAUTION: Never leave any ports open to the air, as sudden suction could result in air entrainment and the subsequent air embolus will be delivered to the patient. Bleeding is a common complication following CentriMag system placement and should be carefully monitored. Excessive bleeding that does not decrease may require a reoperation. Constant attention must be given to maintaining a normal hemoglobin concentration. Excessive diuresis in the post-operative phase should also be carefully monitored, and replacement volume administered as required. Inotropic support is often used to support ventricular function, maintain wall motion, and reduce the risk of intra-ventricular thrombosis, but should be used conservatively during CentriMag system support. High doses or prolonged use of inotropes may deplete myocardial energy stores, making weaning and complete recovery more difficult. Milrinone is the usual drug of choice because of its positive inotropic and vasodilatation effects. Inotropic support should be avoided during the initial weaning and assessments of recovery, but gradually increased during the CentriMag system explant. The pulmonary vascular resistance should be carefully monitored and treated when necessary. Because the PVR is not continuously monitored, acute changes may not be observed. A sudden decrease in the LVAD flow is often caused by inadequate intra-ventricular volume but may also be an indication of an elevated PVR due to administration of blood products, a response to an infusion, or other cause. Pulmonary vasodilators are commonly used in the immediate postoperative period, with inhaled nitric oxide being the most effective and safe. Patients with significant bleeding that require transfusions may be expected to have an increase in PVR. Many CentriMag system users apply prophylactic nitric oxide and use intravenous vasodilators as a last resort.
Intra-aortic Balloon Pump An intra-aortic balloon pump may provide pulsatility during CentriMag system support, but its usefulness with the CentriMag system has not been demonstrated. If used with LVAD support, the augmentation or balloon volume should be decreased so that complete occlusion of the aorta does not occur. Consider pulling back the sheath to improve distal perfusion, which should be assessed at least hourly. The IABP may be removed in the critical care unit after coagulation parameters have normalized. If weaning is anticipated within 48 to 72 hours, leaving the IABP in place may be appropriate.
Defibrillation/ Cardioversion Defibrillation or cardioversion may be necessary during severe arrhythmias. Cardioversion may be performed without stopping the pump. Ensure that a backup console and motor are available, powered and in the immediate vicinity. If cardioversion is attempted without discontinuing support, consideration should be given to reducing the speed of the pump (or pumps for BiVAD support) to reduce the likelihood of Right-Left imbalance and pump inlet obstruction. Following cardioversion, slowly increase the speed (or resume BiVAD support) while monitoring the patient's hemodynamics to ensure adequate volume available for the desired flow. CAUTION: If you choose to reduce the speed during cardioversion, carefully monitor systemic hemodynamics for adequate
17
perfusion, and immediately increase the speed to reach target flow when cardioversion is complete.
Anticoagulation Generally, no anticoagulation therapy is used in the first 6 to 24 hours after initiation of support due to usual postoperative bleeding. Cases where CPB was not used prior to initiation of support, and bleeding is minimal, low dose anticoagulation with heparin should be started sooner. Pump thrombosis may be minimized by maintaining flow of at least 3.0 LPM. Intravenous heparin is usually started after the chest tube drainage is less than 50 ml/hour for at least 2 to 3 hours. The initial target ACT is 160-180 seconds, the target PTT is 1.3-1.6 times the laboratory normal, or the anti-Xa assay shows 0.3-0.7 IU/mL. As anticoagulation and hemostasis may be affected by end organ function, platelet levels, platelet function, CentriMag system flow, native cardiac output, and other factors, anticoagulation must be individualized for each patient by the attending physicians. CAUTION: Monitor and administer anticoagulation carefully, as risk of bleeding or thrombosis may occur with inappropriate management. Heparin-induced thrombocytopenia is a complication of heparin therapy that presents with bleeding and consumption of platelets. Treatment for HIT consists of withholding or reversing heparin. Aspirin, bivalirudin, warfarin, and a variety of other anticoagulants may be considered as alternatives to heparin, depending on clinical objectives, experience at the individual center, and hepatic and/or renal function. Existing institutional protocols for managing HIT should be implemented as appropriate. A hematology consult can also be valuable in the management of these patients. Thromboelastography is used by some centers for the management of anticoagulation. Its use for VAD patients is not universally accepted, although some centers with TEG equipment, experienced personnel, and well-defined protocols have found it useful and reliable. If TEG is used, teams should be trained to ensure consistent results. The TEG should be initially reviewed carefully every day to assess antiplatelet needs until stable and satisfactory levels are achieved. Anticoagulation needs vary by patient and should be adjusted based on clinical judgment.
Wound Care If the cannulas are tunneled, postoperative wound care should be consistent with standard surgical protocols. A standard occlusive dressing should be used at the surgical sites to minimize the risk of infection. Cannula exit sites should be under a separate dressing from the chest tube exit sites if possible. Aseptic technique should be used by all staff when handling the surgical sites during dressing changes and other wound care. The importance of consistent hand washing practices by staff and caretakers cannot be overemphasized. Wound sites should be carefully inspected for signs of tissue breakdown or excessive drainage. Undue pressure or torque to the surgical site should be avoided in order to minimize trauma with special care to secure the wound site taken during patient ambulation or transportation.
Nutrition Enteral or parenteral feeding should be implemented when feasible during support. It is important that patients who achieve explantation receive proper nutritional education from the hospital nutritionist to optimize recovery.
Physical Therapy When feasible, the patient should receive passive and active range of motion physical therapy as tolerated. Some patients have also been able to ambulate during CentriMag system support. Should ambulation be considered, care must be taken to protect the cannulas, tubing and pump from any kinks or tension on the circuit. It is advisable to ensure additional securing features (i.e., bands) on all connection sites of the circuit. Furthermore, if ambulation is considered ensure that there is an appropriate number of staff available to monitor and support both patient and circuitry. Before movement of the patient or circuit, inspect all connections of the circuit to be sure they are intact. CAUTION: Ensure that the length of the tubing is adequate for ambulation to avoid the risk of disconnection, cannula migration, or dislodgement. Bedside range of motion or other light exercise is possible with extreme care, and useful for patients on support for multiple weeks.
Patient Transport In some cases, a patient on CentriMag system support may need to be transported to another location within the hospital or to another medical center. The CentriMag system meets international standards for air and ground transport and is designed for ease of use during transport between medical centers. The system has been designed for portability in acute and critical care situations. When transporting a patient within the hospital, consider the following:
Care must be taken to avoid dislodgement or disconnection of the cannula and tubing connections. The pump and motor unit should be on a stable cart or placed in the bed with the patient and secured, or placed in the CentriMag system transporter which has been attached to the bed. If the motor is placed on the patient’s bed, the cable length from the console to the motor is usually sufficient to transport the console on its cart alongside of the patient’s bed. If the motor is placed on the patient’s bed, ensure that the pump and tubing are visible at all times. If necessary, the console can be detached from its cart and placed on the bed. Because of the weight of the motor and the console, these items should not be placed on top of the patient. The motor, when operating, is warm to the touch. A barrier between the motor and the patient can be used to ensure that heat from the motor does not come in contact with the patient’s skin. CAUTION: Do not cover the motor or console with blankets to prevent them from overheating.
18
In the event that the patient is being transported to another medical center, the transport process involves three teams: the transferring (spoke) center team; air or ground transport team; and the receiving (hub) center team. Key priorities include pretransport coordination, maintaining hemodynamic support, and continuous monitoring of the patient’s hemodynamics and CentriMag system flow.
Transport Protocols Existing institutional protocols for IABP, cardiopulmonary support, or ventilator- dependent patient transport may serve as useful templates for institutional CentriMag system transport protocols. Transport protocols should include:
Equipment and supplies needed Individuals and responsibilities Primary and backup power sources Securing of equipment during transport Response to most likely complications
Transporting a patient on CentriMag system support requires a team approach for the best results. Some guidelines to follow include:
Identify and communicate with the receiving or hub hospital in advance. Assign one individual to monitor the circuit, consoles and pumps who will be prepared to make system adjustments as needed during transport. CAUTION: There is increased risk of air entrainment when the patient is being moved, particularly when the patient’s chest has not been fully closed.
Pre-position equipment and supplies. Load all backup equipment and supplies into the transport vehicle before loading the patient. Ensure that the pumps and motors are not covered, and that an additional console, motor and tubing clamps are always with the patient. The equipment should be secured to the gurney, stretcher or transport vehicle with appropriate straps or fixtures to prevent movement during transport, for both intra- and inter-hospital transport. The console has 2 hours of battery power. Ensure that there is another console fully charged with a motor attached in immediate vicinity of the patient during transport. Prior to shutting off the power supply and removal of the patient from the transport vehicle, briefly unplug the console’s power cord to confirm adequate battery charge and console operation.
For details on the equipment as well as FAA and other standards for transport, refer to the CentriMag Circulatory Support System Operation Manual.
Prevention and Management of Potential Complications Potential complications are similar to those seen with other ventricular assist devices. Flow disruption is the most common complication and can result from hypovolemia, obstruction or malposition of the cannulas, right ventricular failure, cardiac tamponade, and/or arrhythmia. In these cases, increasing the RPM may result in an exacerbation of the complication, or accelerated decrease in VAD flow. This should alert the operator to immediately reduce the RPM, diagnose, and address the underlying condition causing the complication. Patients should be carefully and frequently assessed for complications listed in the table below. Table 5. Prevention and management of potential complications Complication
Prevention and management
Low flow or inflow obstruction
Decrease RPM. Monitor pressures and flow. Rule out and correct hypovolemia, tamponade, and/or obstruction or malposition of cannula.
Right ventricular dysfunction
Rule out and, if possible, adjust VAD flows, vasodilators, and/or inotropes to correct an intra- ventricular septal shift toward the left ventricle.
Increased pulmonary vascular resistance
Consider pulmonary vasodilators or mechanical right ventricular RVAD support. Minimize fluids and transfusions as feasible. Hyperventilate. Consider pulmonary vasodilators.
Patent foramen ovale with shunting
Repair defect if feasible. If not feasible, reduce or eliminate shunting by adjusting VAD flow and pharmacological support to maintain RAP > LAP.
Bleeding at cannulation and other sites
Use meticulous technique during surgery and cannulation. Secure the cannulas with dual purse-string pledgeted sutures. Minimize postoperative patient movement. Monitor anticoagulation and hemostasis status.
19
Table 5. Prevention and management of potential complications Complication
Prevention and management
Thrombus formation within the heart, circuit or system components
Assess thrombi with TEE for stability; and remove during surgery or address with appropriate anticoagulation. Delay weaning, if necessary, until resolved. Avoid conditions which can cause suction or line chatter. Avoid flexing the tubing, particularly near the connectors, which can dislodge fibrin or deposits.
Hemolysis
Troubleshoot to identify cause: cannula position, cannula selection, CVVH, oxygenator, kinked tubing, another device, high RPM/flow. Check that pump is mounted properly. Consider pump change if suspect as a final option.
Pump not inserted correctly
Mount the pump correctly. Change pump if incorrect mount is accompanied by platelet consumption &/or hemolysis.
Console or motor malfunction
Switch pump to backup console and motor. Document, replace, and report.
Decannulation
Prevent by securing the cannulas to the tissue at multiple sites following cannulation. Minimize postoperative patient and circuit movement. Use extreme care when moving the patient.
Air entrainment and embolism
Immediately clamp pump outlet tubing. Stop pump. Depending on circumstances and anticoagulation, consider splicing in a connector, deairing, and/or pump exchange.
Alarms/Alerts and Troubleshooting For information on alarms and alerts, refer to the CentriMag Circulatory Support System Operation Manual.
Weaning and Explantation Recovery sufficient for removal from CentriMag system support will depend on specific patient hemodynamic status. Depending on the extent of myocardial injury: Patients may recover sufficiently to be weaned within 48 to 72 hours. Patients may require support for multiple weeks. Patients may not recover sufficiently to be weaned from support and will required long-term support with an implantable LVAD or heart transplant. Improvement in ventricular function is usually first noted with increased contractility and ventricular ejection apparent on the arterial pressure waveform, decreased flow required to maintain patient hemodynamics, and a decreased dependence on inotropic support. Initial assessments of ventricular function should be made without increasing inotropic support, IABP support, or without volume loading of the ventricles. Echocardiography is useful to assess improvement in ventricular size, wall motion and ejection fraction. When possible, a pulmonary artery catheter provides useful information on recovery. Recovery is based on the patient’s ability to maintain hemodynamic status, perfusion, and end organ function during extended period of low CentriMag system flow without additional pharmacological or mechanical support. CAUTION: There is a risk of thrombosis if the pump flow is reduced without adequate anticoagulation. Before you reduce the pump speed, allow time for adequate anticoagulation circulation. CAUTION: If the drainage or return cannula is placed directly in the heart (left or right atria or ventricles), then the removal of blood from the heart will unload the heart and reduce the amount of blood flowing through the ventricular outflow (pulmonary or aortic) valves. A trial period of CentriMag system weaning over at least three hours may be attempted after the following criteria are met:
Hemodynamic evidence of ventricular function improvement based on increased cardiac output Increase in mean arterial blood pressure Documented pressure, echocardiographic evidence, or TEE evidence of ventricular ejection with little or no inotropic support
Initial attempts to wean should be short in duration with an appropriate increase in anticoagulation and gradual reduction in pump flow to 1.5 to 2.0 liters per minute. If the ventricles become visibly dilated on TEE, mixed venous oxygen saturation is compromised, or the patient's hemodynamic parameters deteriorate, the weaning attempt should be discontinued. Once weaning is successful, expect increased pharmacological support to be required. WARNING: After you wean the patient from support, closely monitor their hemodynamics for deterioration, as this may require emergent re-initiation of support.
Weaning Protocol The most appropriate timing for weaning CentriMag system support has not been determined and there are no specific criteria. Key parameters to assess for weaning are ventricular contractility and ejection. As the heart recovers function, the pulse pressure on the
20
arterial pressure tracing will increase. Serial echocardiography to assess contractility and ejection fraction provides a good indication of ventricular recovery. Decreased dependence on inotropic drugs is an important indicator of recovery. Guidelines for weaning a patient from and termination of CentriMag system support include: 1.
Final weaning and termination is preferentially done in an operating room.
2.
Transesophageal echocardiography should be used continuously to assess ventricular function. Observe for ventricular dilation, septal shift, ejection fraction, and changes in inotropic drug requirements.
3.
Decrease the flow rate by 0.5 LPM every 15-30 minutes until 2.0 LPM is reached.
4.
Increase anticoagulation to a target ACT > 300 seconds.
5.
Continue weaning as above until flow rate is 0.5 LPM.
6.
Clamp the return tubing to terminate support, decrease the set speed to zero, and continue to carefully monitor the patient’s hemodynamics and perfusion.
7.
If the patient remains stable on low dose inotropic support, decannulate.
8.
Consider using an IABP and/or leaving the sternum unwired (skin closure only) for patients with marginal function following decannulation.
Pump Exchange Pump exchange may be necessary if the duration of support exceeds the indicated duration for use, if hemolysis is believed to be caused by the pump, or if there are indications of thrombosis at the inlet or outlet of the pump or inside the pump. A pump may be exchanged using the following procedure: 1.
Using a sterile field and aseptic technique, a new pump or pump and circuit are primed as described in the Preparing for CentriMag System Use section. Tubing connectors are placed at the patient ends of the tubing. It is always advisable to change the pump as well as the tubing, rather than the pump alone. CAUTION: Ensure that the patient is adequately pharmacologically supported before discontinuing CentriMag system support, as the patient's arterial pressure may drop upon discontinuation of support.
2.
Four tubing clamps are used to clamp the patient’s existing drainage and return tubing.
3.
After the clamps are placed, the pump speed setting on the console is turned to zero.
4.
The existing tubing is cut at least 4-5 cm from the cannula-connector end.
5.
The new tubing connectors are attached using a wet-wet connection while taking care to eliminate air at the junction as well as in the circuit. Secure these new connections with bands.
6.
Ensure that the pump is securely inserted into the motor, and that the pin is screwed in.
7.
Turn the CentriMag system set speed to >1000 RPM, and remove clamps. Increase the set speed to achieve target flow.
Explantation Before device removal, ensure adequate volume and anticoagulation levels, particularly if the pump is going to be run with low flow (under 2 liters per minute) for any length of time. If available, use TEE to check for the presence of thrombi in the atria, ventricles, and at the cannulation sites prior to weaning and device removal. Explantation generally requires a repeat sternotomy. During decannulation, the surgeon should allow retrograde bleeding from the cannulation site to remove any thrombus that may have formed at the cannula site. During periods when the heart is being manipulated, the CentriMag system set speed should be reduced. If flow is compromised by manipulation of the heart, immediately reduce the set speed or clamp the return tubing as necessary to prevent inflow obstruction and/or air entrainment. CAUTION: Abrupt changes in the CentriMag system flow due to manipulation of the heart may result in air entrainment.
Summary of Clinical Experience The clinical study experience for the CentriMag system includes four FDA-approved, prospective, non-randomized, multi-center, unblended, controlled studies encompassing 95 patients. The clinical studies are: 1.
Cardiogenic Shock Pilot Trial [CentriMag VAS Cardiogenic Shock Trial] (IDE G030052)
2.
RVAS Pilot Study [CentriMag VAS: Use as an RVAS Following Implantation of a Commercially Approved LVAS] (IDE G040029)
3.
Pivotal Study [CentriMag VAS Failure to Wean (FTW) from Cardiopulmonary Bypass Trial] (IDE G030052/S21)
4.
HDE PAS Study [CentriMag RVAS U.S. Post Approval Study (PAS)] (H070004)
Data from these clinical studies, together with the results of a comprehensive literature review and an analysis of global postmarket surveillance data, are the basis for the CentriMag system clinical experience overview. Because the pivotal study (IDE G030052/S21) was the only study to strictly enroll and analyze outcomes for the study population reflected in the indication for use in this PMA, it was the only one used to assess effectiveness of the device for this PMA. However, because adverse events
21