BBraun
Insertion instrument for hip endoprosthesis stems
31 Pages
Preview
Page 1
Note Mechanical reprocessing should be favored over manual cleaning as it gives better and more reliable results.
Aesculap® Insertion instrument for hip endoprosthesis stems
Note Successful processing of this medical device can only be ensured if the processing method is first validated. The operator/sterile processing technician is responsible for this. The recommended chemistry was used for validation.
Legend
Note If there is no final sterilization, then a virucidal disinfectant must be used.
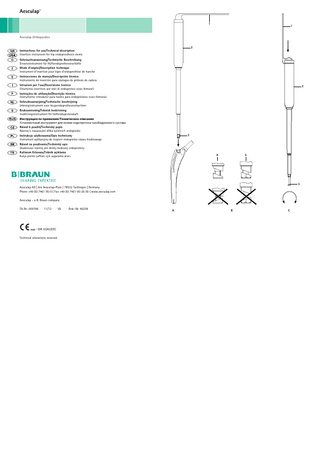
1 2 3 4 5
Note For the latest information on reprocessing and material compatibility see also the Aesculap extranet at www.extranet.bbraun.com The validated steam sterilization procedure was carried out in the Aesculap sterile container system.
Clamping lever Handle Tensioning wedge Polygon adapter Hexagon adapter
General information
Symbols on product and packages Caution, general warning symbol Caution, see documentation supplied with the product
Intended use The insertion instrument is used for implanting hip endoprosthesis stems, using an appropriate adapter intended for this purpose. Observe the instructions for use of the implant. The insertion instrument allows rotation-free adaptation, positioning and implantation of the implant. The insertion instrument is separated from the implant without stress on the implant environment and the implant Due to the limited pulling strength of the instrument, it can not be used for explanting the prosthesis stem.
Safe handling and preparation CAUTION Federal law restricts this device to sale by, or on order of a physician! ► Ensure that the product and its accessories are operated and used only by persons with the requisite training, knowledge, or experience. ► Read, follow, and keep the instructions for use. ► Use the product only in accordance with its intended use, see Intended use. ► Remove the transport packaging and clean the new product, either manually or mechanically, prior to its initial sterilization. ► Store any new or unused products in a dry, clean, and safe place. ► Prior to each use, inspect the product for loose, bent, broken, cracked, worn, or fractured components. ► Do not use the product if it is damaged or defective. Set aside the product if it is damaged. ► Replace any damaged components immediately with original spare parts.
Dried or affixed surgical residues can make cleaning more difficult or ineffective and lead to corrosion. Therefore the time interval between application and processing should not exceed 6 h; also, neither fixating pre-cleaning temperatures >45 °C nor fixating disinfecting agents (active ingredient: aldehydes/alcohols) should be used. Excessive measures of neutralizing agents or basic cleaners may result in a chemical attack and/or to fading and the laser marking becoming unreadable visually or by machine for stainless steel. Residues containing chlorine or chlorides e.g. in surgical residues, medicines, saline solutions and in the service water used for cleaning, disinfection and sterilization will cause corrosion damage (pitting, stress corrosion) and result in the destruction of stainless steel products. These must be removed by rinsing thoroughly with demineralized water and then drying. Additional drying, if necessary. Only process chemicals that have been tested and approved (e.g. VAH or FDA approval or CE mark) and which are compatible with the product’s materials according to the chemical manufacturers’ recommendations may be used for processing the product. All the chemical manufacturer's application specifications must be strictly observed. Failure to do so can result in the following problems: ■ Optical changes of materials, e.g. fading or discoloration of titanium or aluminum. For aluminum, the application/process solution only needs to be of pH >8 to cause visible surface changes. ■ Material damage such as corrosion, cracks, fracturing, premature aging or swelling. ► Do not use metal cleaning brushes or other abrasives that would damage the product surfaces and could cause corrosion. ► Further detailed advice on hygienically safe and material-/value-preserving reprocessing can be found at www.ak-i.org, link to Publications, Red Brochure – Proper maintenance of instruments.
Disassembling the product before carrying out the reprocessing procedure ► Disassemble the product immediately after use, as described in the respective instructions for use.
Preparations at the place of use ► If applicable, rinse non-visible surfaces preferably with deionized water, with a disposable syringe for example. ► Remove any visible surgical residues to the extent possible with a damp, lint-free cloth. ► Transport the dry product in a sealed waste container for cleaning and disinfection within 6 hours.
Preparation before cleaning
Safe operation
► Dismantle the product prior to cleaning, see Disassembling.
Risk of injury and/or malfunction! ► Always carry out a function check prior to using the product.
Cleaning/disinfection Product-specific safety notes on the reprocessing procedure
WARNING Risk of injury when using the product beyond the field of view! ► Apply the product only under visual control. WARNING
CAUTION
Important notes ► To ensure that clamping lever 1 can be opened after insertion, make certain that the insertion instrument is cor-
rectly positioned on the prosthesis.
Damage to the product due to inappropriate cleaning/disinfecting agents and/or excessive temperatures! ► Use cleaning and disinfecting agents according to the manufacturer’s instructions which – are approved for use, for example, on aluminum, plastic materials, and high-grade steel, – do not attack softeners (e.g. in silicone). ► Observe specifications regarding concentration, temperature and exposure time. ► Do not exceed the maximum permitted cleaning temperature of 60 °C.
► Remove the insertion instrument as soon as the implant has been inserted.
Implantation ► Move clamping lever 1 of the insertion instrument to adapting position (90°), see Fig. A. ► Insert the insertion instrument in the implant port as far as it will go. ► Move clamping lever 1 to touch handle 2 so that the implant is clamped in the insertion instrument.
The implant is automatically set in axial alignment with the insertion instrument. ► To separate the insertion instrument from the implant: Open clamping lever 1 and detach the insertion instrument in the direction of the stem.
Validated cleaning and disinfection procedure Validated procedure
Specific requirements
Reference
Manual cleaning with immersion disinfection
■ Cleaning brush, e.g. TA006874 ■ 20 ml disposable syringe ■ When cleaning instruments with
Chapter Manual cleaning/disinfection and sub-chapter:
movable hinges, ensure that these are in an open position and, if applicable, move the joint while cleaning.
Disassembling
► Insert clamping lever 1 in handle 2 and mildly press on it in assembly position, see Fig. C. ► From the lower end of the instrument, insert tensioning wedge 3 in the insertion instrument and turn it to the
or medical compressed air Manual pre-cleaning with brush and subsequent mechanical alkaline cleaning and thermal disinfection
■ Cleaning brush, e.g. TA006874 ■ 20 ml disposable syringe ■ Place the instrument in a tray that is suitable for cleaning (avoiding rinsing blind spots).
right as far as it will go. In this way tensioning wedge 3 is fastened. ► Align the beveled surfaces of tensioning wedge 3 and move clamping lever 1 beyond the ratchet resistance to its adaption position, see Fig. B.
■ Connect components with lumens and channels directly to the rinsing port of the injector carriage.
Chapter Mechanical cleaning/disinfection with manual pre-cleaning and sub-chapter:
■ Chapter Manual pre-cleaning with a brush
■ Chapter Mechanical alkaline cleaning and thermal disinfecting
■ Place instruments in the tray with
Note If there is no noticeable ratchet resistance, the tensioning wedge needs to be tightened further.
Validated reprocessing procedure
immersion disinfection
■ Drying phase: Use a lint-free cloth
► Move clamping lever 1 beyond a ratchet resistance to its assembly position (180°), see Fig. C. ► To release tensioning wedge 3, turn it to the left and remove it downward. ► Pull out clamping lever 1 from handle 2.
Assembling
■ Chapter Manual cleaning with
their hinges open.
Manual cleaning/disinfection ► Prior to manual disinfecting, allow water to drip off for a sufficient length of time to prevent dilution of the dis-
General safety instructions Note Adhere to national statutory regulations, national and international standards and directives, and local, clinical hygiene instructions for sterile processing. Note For patients with Creutzfeldt-Jakob disease (CJD), suspected CJD or possible variants of CJD, observe the relevant national regulations concerning the reprocessing of products.
infecting solution. ► After manual cleaning/disinfection, check visible surfaces visually for residues. ► Repeat the cleaning /disinfection process if necessary.
Manual cleaning with immersion disinfection
Mechanical alkaline cleaning and thermal disinfecting Machine type: single-chamber cleaning/disinfection device without ultrasound
Phase
Step
T [°C/°F]
t [min]
Conc. [%]
Water quality
Chemical
I
Disinfecting cleaning
RT (cold)
>15
2
D–W
Aldehyde-free, phenol-free, and QUAT-free concentrate, pH ~ 9*
II
Intermediate rinse
RT (cold)
1
-
D–W
-
III
Disinfection
RT (cold)
15
2
D–W
Aldehyde-free, phenol-free, and QUAT-free concentrate, pH ~ 9*
IV
Final rinse
RT (cold)
1
-
FD-W
-
V
Drying
RT
-
-
-
-
D–W: FD–W:
Drinking water Fully desalinated water (demineralized, low microbiological contamination: drinking water quality at least) RT: Room temperature *Recommended: BBraun Stabimed ► Note the information on appropriate cleaning brushes and disposable syringes, see Validated cleaning and dis-
infection procedure. Phase I ► Fully immerse the product in the cleaning/disinfectant for at least 15 min. Ensure that all accessible surfaces are moistened. ► Clean the product with a suitable cleaning brush in the solution until all discernible residues have been removed from the surface. ► If applicable, brush through non-visible surfaces with an appropriate cleaning brush for at least 1 min. ► Mobilize non-rigid components, such as set screws, links, etc. during cleaning. ► Thoroughly rinse through these components with the cleaning disinfectant solution (at least five times), using a disposable syringe. Phase II ► Rinse/flush the product thoroughly (all accessible surfaces) under running water. ► Mobilize non-rigid components, such as set screws, joints, etc. during rinsing. ► Drain any remaining water fully.
Phase IV ► Rinse/flush the product thoroughly (all accessible surfaces). ► Mobilize non-rigid components, such as set screws, joints, etc. during final rinse. ► Rinse lumens with an appropriate disposable syringe at least five times. ► Drain any remaining water fully.
Note The cleaning and disinfection device must be of tested and approved effectiveness (e.g. FDA approval or CE mark according to DIN EN ISO 15883). Note The cleaning and disinfection device used for processing must be serviced and checked at regular intervals.
Manual pre-cleaning with a brush Phase
Step
T [°C/°F]
t [min]
Conc. [%]
Water quality
Chemical
I
Disinfectant cleaning
RT (cold)
>15
2
D–W
Aldehyde-free, phenol-free, and QUAT-free concentrate, pH ~ 9*
Rinsing
RT (cold)
D–W
t [min]
Water quality
Chemical
I
Prerinse
<25/77
3
D–W
-
II
Cleaning
55/131
10
FD-W
■ Concentrate, alkaline: – pH = 13 – <5 % anionic surfactant
■ 0.5 % working solution – pH = 11* III
Intermediate rinse
>10/50
1
FD-W
-
IV
Thermal disinfecting
90/194
5
FD-W
-
V
Drying
-
-
-
According to the program for cleaning and disinfection device
D–W: FD–W:
Drinking water Fully desalinated water (demineralized, low microbiological contamination: drinking water quality at least) *Recommended: BBraun Helimatic Cleaner alkaline ► Check visible surfaces for residues after mechanical cleaning/disinfecting.
Inspection, maintenance and checks
CAUTION
Damage (metal seizure/friction corrosion) to the product caused by insufficient lubrication! ► Prior to function checks, lubricate moving parts (e.g. joints, pusher components and threaded rods) with maintenance oil suitable for the respective sterilization process (e.g. for steam sterilization: Aesculap STERILIT® I oil spray JG600 or STERILIT® I drip lubricator JG598).
and free of damage (e.g. broken insulation or corroded, loose, bent, broken, cracked, worn, or fractured components). ► Dry the product if it is wet or damp. ► Repeat cleaning and disinfection of products that still show impurities or contamination. ► Check that the product functions correctly. ► Immediately put aside damaged or inoperative products and send them to Aesculap Technical Service, see Technical Service. ► Assemble dismountable products, see Assembling. ► Check for compatibility with associated products.
► Place the product in its holder or on a suitable tray. Ensure that all cutting edges are protected. ► Pack trays appropriately for the intended sterilization process (e.g. in sterile Aesculap containers). ► Ensure that the packaging provides sufficient protection against recontamination of the product during storage.
Steam sterilization
Mechanical cleaning/disinfection with manual pre-cleaning
-
T [°C/°F]
Packaging
Phase V ► Dry the product in the drying phase with suitable equipment (e.g. cloth, compressed air), see Validated cleaning and disinfection procedure.
1
Step
► Allow the product to cool down to room temperature. ► After each complete cleaning, disinfecting and drying cycle, check that the instrument is dry, clean, operational,
Phase III ► Fully immerse the product in the disinfectant solution. ► Mobilize non-rigid components, such as set screws, joints, etc. during rinsing. ► Rinse lumens at least 5 times at the beginning of the exposure time using an appropriate disposable syringe. Ensure that all accessible surfaces are moistened.
II
Phase
-
Note The product may only be sterilized when dismantled. ► Check to ensure that the sterilizing agent will come into contact with all external and internal surfaces (e.g. by
opening any valves and faucets). ► Validated sterilization process
– Disassemble the instrument – Steam sterilization through fractionated vacuum process – Steam sterilizer according to DIN EN 285 and validated according to DIN EN ISO 17665 – Sterilization using fractionated vacuum process at 134 °C/holding time 5 min ► When sterilizing several instruments at the same time in a steam sterilizer, ensure that the maximum load capacity of the steam sterilizer specified by the manufacturer is not exceeded.
Sterilization for the US market ■ Aesculap advises against sterilizing the device by flash sterilization or chemical sterilization. ■ Sterilization may be accomplished by a standard prevacuum cycle in a steam autoclave. To achieve a sterility assurance level of 10-6 , Aesculap recommends the following parameters:
D–W: Drinking water RT: Room temperature *Recommended: BBraun Stabimed ► Note the information on appropriate cleaning brushes and disposable syringes, see Validated cleaning and dis-
infection procedure. Phase I ► Fully immerse the product in the cleaning/disinfectant for at least 15 min. Ensure that all accessible surfaces are moistened. ► Clean the product with a suitable cleaning brush in the solution until all discernible residues have been removed from the surface. ► If applicable, brush through non-visible surfaces with an appropriate cleaning brush for at least 1 min. ► Mobilize non-rigid components, such as set screws, links, etc. during cleaning. ► Thoroughly rinse through these components with the cleaning disinfectant solution (at least five times), using a disposable syringe. Phase II ► Rinse/flush the product thoroughly (all accessible surfaces) under running water. ► Mobilize non-rigid components, such as set screws, joints, etc. during rinsing.
Aesculap Orga Tray/Sterile container (perforated bottom) Minimum cycle parameters* Sterilization method
Temp.
Time
Minimum drying time
Prevacuum
270 °F/275 °F
4 min
20 min
*Aesculap has validated the above sterilization cycle and has the data on file. The validation was accomplished in an Aesculap sterile container cleared by FDA for the sterilization and storage of these products. Other sterilization cycles may also be suitable, however individuals or hospitals not using the recommended method are advised to validate any alternative method using appropriate laboratory techniques. Use an FDA cleared accessory to maintain sterility after processing, such as a wrap, pouch, etc.
Storage ► Store sterile products in germ-proof packaging, protected from dust, in a dry, dark, temperature-controlled area.
Technical Service Risk of injury and/or malfunction! ► Do not modify the product. WARNING ► For service and repairs, please contact your national B. Braun/Aesculap agency.
Modifications carried out on medical technical equipment may result in loss of guarantee/warranty rights and forfeiture of applicable licenses. Service addresses Aesculap Technischer Service Am Aesculap-Platz 78532 Tuttlingen / Germany Phone: +49 (7461) 95-1602 Fax: +49 (7461) 16-5621 E-Mail: [email protected] Or in the US: Aesculap Implant Systems LLC Attn. Aesculap Technical Services 615 Lambert Pointe Drive Hazelwood MO, 63042 Aesculap Repair Hotline Phone: +1 (800) 214-3392 Fax: +1 (314) 895-4420 Other service addresses can be obtained from the address indicated above.
Disposal ► Adhere to national regulations when disposing of or recycling the product, its components and its packaging!
Distributor in the US/Contact in Canada for product information and complaints Aesculap Implant Systems LLC 3773 Corporate Parkway Center Valley, PA, 18034, USA TA-Nr. 009788
11/12
V6
Änd.-Nr. 46258