BBraun
PAS-Port Proximal Anastomosis System and Vein Aorta Gauge
61 Pages
Preview
Page 1
Aesculap®
1
2
1a
Aesculap Surgical Instruments
en USA
de fr es it pt nl sv ru cs pl sk tr
Instructions for use/Technical description PAS-Port Proximal Anastomosis System and Vein/Aorta Gauge Note for U.S. users This Instructions for Use is NOT intended for United States users. Please discard. The Instructions for Use for United States users can be obtained by visiting our website at www.aesculapusa.com. If you wish to obtain a paper copy of the Instructions for Use, you may request one by contacting your local Aesculap representative or Aesculap's customer service at 1-800-282-9000. A paper copy will be provided to you upon request at no additional cost. Gebrauchsanweisung/Technische Beschreibung PAS-Port Proximales Anastomosensystem und Venen-/Aortenlehre Mode d’emploi/Description technique Système d’anastomose proximale PAS-Port et jauge de veine/aorte Instrucciones de manejo/Descripción técnica Sistema de anastomosis proximal PAS-Port y cánula venosa/aórtica Istruzioni per l’uso/Descrizione tecnica PAS-Port sistema per anastomosi prossimale e calibro vena/aorta Instruções de utilização/Descrição técnica Sistema de anastomoses proximal PAS-Port e calibre de veias e aortas Gebruiksaanwijzing/Technische beschrijving PAS-Port proximaal anastomotisch systeem en ader-/aortamal Bruksanvisning/Teknisk beskrivning PAS-Port proximalt anastomossystem och ven-/aortaprob Инструкция по примению/Техническое описание Система для проксимального анастомоза и шаблон для вен/аорты PAS-Port Návod k použití/Technický popis Systém PAS-Port pro proximální anastomózu a žilní/aortální měřítko Instrukcja użytkowania/Opis techniczny System anastomozy proksymalnej PAS-Port oraz sprawdzian żylny/tętniczy Návod na použitie/Technický opis Systém proximálnej anastomózy a pomôcka na určenie veľkosti aorty/žíl PAS-Port Kullanım Kılavuzu/Teknik açiklama PAS-Port proksimal anastomoz sistemi ve toplardamar/aort sizer
5a
5
4
3b
2
3a
3a
1b
1
1g
1f
1e
6a 6b
6
6c 6c
Aesculap AG | Am Aesculap-Platz | 78532 Tuttlingen | Germany Phone +49 (0) 7461 95-0 | Fax +49 (0) 7461 95-26 00 | www.aesculap.com Aesculap® – a B. Braun brand TA015510
2020-05
V6
1c
Change No. 63066
A
B
5b
3b
0482
C
E
G
D
3b
2
3b
2
3b
3b
F
3b
H
3b
1g 1f
I
1g
J
1d
en ®
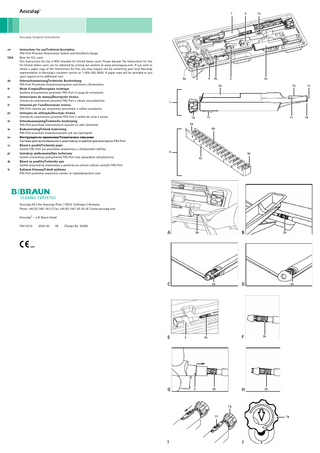
Aesculap PAS-Port Proximal Anastomosis System and Vein/Aorta Gauge PAS-Port Proximal Anastomosis System 1 Delivery Tool 1a Guide Clip 1b Seal Housing 1c Auger Tip (bar drill) 1d Deployment End 1e Opening - Orient Toward Surgeon 1f Safety Switch 1g Knob (Knob End) 2 Poke-Through Tool (2×) 3 Cartridge with Anastomosing Implant 3a Cartridge 3b Anastomosing Implant 4 Stop Clip 5 Pull-Through Tool 5a Releaser 5b Wire hook 6 Vein/Aorta Gauge 6a Target Vessel Slot 6b Conduit Outside Diameter Slots 6c Conduit Double Wall Thickness Slots
About this document
Note General risk factors associated with surgical procedures are not described in these instructions for use.
1.1
Scope
These instructions for use apply for the following products: Art. no.
Designation
FC700SU
PAS-Port Proximal Anastomosis System
FC705
Vein/Aorta Gauge
► For item-specific instructions for use and information regarding preparation and material compatibility, see also
the Aesculap Extranet at www.extranet.bbraun.com
1.2
Safety messages
Safety messages make clear the dangers to patient, user and/or product that could arise during the use of the product. Safety messages are labeled as follows: DANGER Danger of death or serious injury. WARNING Danger of minor injury or product damage. CAUTION Indicates a possible threat of material damage. If not avoided, the product may be damaged.
2.
Clinical use
2.1
Product description
PAS-Port Proximal Anastomosis System The PAS-Port System delivers an implant designed to create an anastomosis between a large target vessel (e.g. aorta) and small caliber conduit (e.g. saphenous vein). The implant is a self-closing stainless steel clip that will create a complete end-to-side anastomosis that is 4.65 mm in internal diameter when deployed and which is functionally equivalent to a standard hand-sutured anastomosis. The PAS-Port System is contained in a package that is designed to facilitate attachment of the conduit to the implant, as well as to ensure that the conduit (after attachment to the system and before deployment) is kept moist and vital. Vein/Aorta Gauge The Vein/Aorta Gauge (see figure 6) is a product for estimating the outside diameter and wall thickness of a conduit and the outside diameter of a target vessel. The determined value serves only as a reference value.
2.2
Areas of use and limitations of use
2.2.1
Intended use
PAS-Port Proximal Anastomosis System The PAS-Port System is designed to create an anastomosis between a large target vessel, such as the aorta, and a conduit, such as a venous conduit. Vein/Aorta Gauge The Vein/Aorta Gauge is intended to allow reference assessment of graft conduit outside diameter and wall thickness, and the outside diameter of a target vessel, such as the human aorta.
2.2.2
Indications
Note The manufacturer is not responsible for any use of the product against the specified indications and/or the described applications. PAS-Port Proximal Anastomosis System The PAS-Port System is intended to create an everting anastomosis between the aorta and an autologous vein graft. Note The PAS-Port System has not been studied in arterial grafts. Vein/Aorta Gauge ■ The aorta will be assessed in-situ. ■ The graft conduit is assessed ex-situ. ■ The graft conduit diameter is assessed while it is pressurized via syringe to the pressure typically used to detect leaks during preparation for use. ■ The graft conduit wall thickness is assessed across both wall thicknesses at the same time while the graft conduit is flaccid.
2.2.3
► Do not use this product on target vessels less than or equal to 18 mm in outside diameter and with wall thick-
nesses that would not be acceptable for a hand-sewn anastomosis. ► Do not use this product with conduit vessels that would not typically be used for bypass grafting procedures. ► Do not use this product with conduit vessels that have an outside diameter of less than 4.0 mm or greater than
Legend
1.
Note Such determination may also be based upon echocardiographic demonstration of either mural (e.g. calcification) and/or intimal (e.g. plaque, exudates) disease.
Absolute contraindications
► Do not use this product on target vessels where conventional surgical anastomoses would typically not be cre-
ated due to the presence of palpable disease.
6.0 mm, or with double wall thicknesses greater than 1.4 mm. ► Do not use products in patients with foreign-body sensitivity to stainless steel.
2.2.4
Relative contraindications
The following conditions, individual or combined, can lead to delayed healing or compromise the success of the operation: ■ Medical or surgical conditions (e.g. comorbidities) which could hinder the success of the operation. In the presence of relative contraindications, the user decides individually regarding the use of the product.
2.3
Risks, adverse effects and interactions
As part of the legal duty to inform, the following typical risks, interactions and side effects associated with the use of surgical instruments are pointed out. Possible risks, side effects and interactions of the application currently known to the manufacturer are: ■ Difficulty or impossibility of removing the transplant from the product. ■ Product damage, breakage and/or failure ■ Impossibility to complete the anastomosis with the product and resulting necessity to use another product or to perform an alternative treatment. ■ Bleeding, including escape of blood on the anastomosis ■ Thrombus ■ Aortic dissection ■ Vessel injury/tear ■ Aortotomy requiring repair/treatment ■ Transplant failure or insufficient blood flow in the transplant due to damage, thrombosis, stenosis or occlusion ■ Myocardial ischemia and/or myocardial infarction ■ Neurological complications including TIA and/or stroke ■ Infection ■ Allergic reaction ■ Treatment, repeated treatment, surgical intervention and/or re-operation due to one of the aforementioned complications ■ Any of the aforementioned complications with death resulting
2.4
Safety information
2.4.1
Clinical User
General safety information To prevent damage caused by improper setup or operation, and to not compromise the manufacturer warranty and liability: ► Use the product only according to these instructions for use. ► Follow the safety and maintenance instructions. ► Ensure that the product and its accessories are operated and used only by persons with the requisite training, knowledge, or experience. ► Store the new or unused products in a dry, clean and safe place. ► Prior to use, check that the product is in good working order. ► Keep the instructions for use accessible for the user. Note The user is obligated to report all of the severe events in connection with the product to the manufacturer and the competent state authorities in which the user is located. Notes on surgical interventions The medical specialist will make decisions on concrete use based on the warranted properties and technical data. ■ It is the user's responsibility to ensure that the surgical procedure is performed correctly. ■ Appropriate clinical training as well as a theoretical and practical command of all the required operating techniques, including the use of this product, are prerequisites for the successful use of this product. ■ The user has a duty to consult with the manufacturer for information if the preoperative situation regarding use of the product is ambiguous.
2.4.2
Product
Product-specific safety information Pre-clinical tests have shown that the PAS-Port Implant is conditionally MR-compatible. A patient wearing this product can be subjected to a scan in an MR system without risk under the following conditions:
■ Static magnetic field of 3 Tesla at maximum ■ Maximum spatial magnetic field gradient of 1,000 Gauss/cm (10 T/m) ■ Maximum whole-body averaged specific absorption rate (SAR) indicated for MR systems of 4 W/kg per 15 minute scan (that is, per pulse sequence) in the monitored operating mode of the MR system at the first level. Under the defined scan conditions, it is expected that the PAS-Port Implant will experience a maximum temperature increase of 0.9 °C following an uninterrupted scan of 15 minutes in duration (that is, per pulse sequence). In non-clinical tests, the image artefacts caused by the PAS-Port Implant extend about 15 mm beyond the PAS-Port Implant, when the imaging occurs with a gradient-echo pulse sequence and a 3-Tesla MR system. ► Attend appropriate product training before using the product.
Note Contact the national B. Braun/Aesculap representatives to obtain information regarding training. ► Do not use any solutions containing blood or glucose as storage solution for the conduit vessel. ► Ensure that the average arterial pressure equals at least 50 mmHg when attaching the product. ► Leave components of the PAS-Port Proximal Anastomosis System in the inner shell of the packaging while pre-
paring the conduit and fixing the conduit on the Implant. ► Do not remove the PAS-Port Proximal Anastomosis System from the inner shell until the cartridge with conduit
and Implant is to be loaded into the Delivery Tool, see Loading cartridge into Delivery Tool. ► Do not use conduit if valves or lateral branches are located within 15 mm of the end of the conduit to be attached
to the Implant. ► Do not ligate lateral branches of the conduit with clips. ► Do not use conduit if it cannot be pulled through the cartridge by gentle, continuous application of force. ► Do not use conduit if it can only be everted over the Implant with difficulty due to its small size or lack of elas-
ticity. ► Do not touch sharp Auger Tip (bar drill) 1c on the Deployment End 1d. ► Do not release Safety Switch 1f until the conduit is to be applied.
An opening in the target vessel and the anastomosis is automatically created and applied by the PAS-Port Proximal Anastomosis System. ► Do not create an opening in the target vessel prior to using the product. The risk of bending the transplant can be minimized by the following: ■ Careful selection of anastomosis site on target vessel ■ Careful determination of appropriate transplant length ■ Placement of individual retaining sutures along the course of the transplant
2.4.3
Sterility
2.5.5
Non-sterile packaged products Art. no.
Designation
FC705
Vein/Aorta Gauge
The product is delivered in an unsterile condition. ► Clean the new product after removing its transport packaging and prior to its initial sterilization. Sterile products Art. no.
Designation
FC700SU
PAS-Port Proximal Anastomosis System
The product is gamma-sterilized and supplied in sterile packaging. ► Do not use products from open, damaged or contaminated sterile packaging. ► Do not use the product after its use-by date. Single-use products Art. no.
Designation
FC700SU
PAS-Port Proximal Anastomosis System
► Do not reuse the product.
The reprocessing of the product affects its functionality. Risk of injury, illness or death due to soiling and/or impaired functionality of the product. ► Do not reprocess the product.
2.5
Application
2.5.1
Documentation
Each package contains additional labels showing the article number and lot number and the individual serial number of the product. ► Use these labels for documentation in the patient’s file (for the hospital). The surgical procedure has been explained to the patient, and the patient’s consent has been documented.
2.5.2
Harvesting conduit
► Harvest the conduit by means of the normal methods
– – – – –
Carefully remove connective tissue. Ensure that the suture material size used to ligate lateral branches is 4-0 at maximum. Do not use ligature clips to ligate the lateral branches of the section provided as the conduit. Avoid excessively long lateral branches; the ends of the branches remaining in the patient can be clipped. Do not seal (e.g. ligate) the distal end of the conduit before attaching the product.
Note The distal end of the conduit is the end that is to be connected to the coronary artery by the anastomosis. ► Fill the conduit with an acellular physiological solution in order to check the seal and to suppress spasms, accord-
ing to the routine surgical methods.
Loading the conduit into the cartridge of the PAS-Port Proximal Anastomosis System
► To ensure smooth loading via the Cartridge 3, thoroughly moisten the conduit with acellular physiological solu-
tion and flush cartridge with acellular physiological solution through the rear inlet opening. ► Fix conduit to wire hook:
– – – –
Locate wire hook 5b on the end of the Pull-Through Tool. Lay conduit in the groove in the inner shell which is located in front of the wire hook. Place the end of the conduit that is to be connected to the Implant between the wire hooks 5b, see Fig. A. Compress the handle of the Pull-Through Tool 5 until it clicks in. The handle of the Pull-Through Tool may not move during activation for capturing the conduit. – Ensure that the wire hooks securely grasp the conduit. ► Pull the Pull-Through Tool 5 with the attached conduit through the Cartridge 3a. When doing so, ensure that no lateral branches are caught on the inlet opening when advancing the conduit into the cartridge. ► Pull conduit further through the Cartridge 3a until it emerges on the Implant end of the cartridge. The conduit should protrude approx. 8 mm beyond the tip of the Implant. ► Once the conduit has been pulled through the cartridge intact: – Cut off the end of the conduit near the puncture points of the wire hooks 5b. This can be done without releasing the hooks. – Ensure that the conduit does not slip back into the Cartridge 3a after separating. – Ensure that all tissue injured by the hooks is removed, see Fig. B. – The everting end of the conduit should protrude 3 to 6 mm beyond the tip of the Implant. ► Put Pull-Through Tool 5 aside. Remove Stop Clip 4 from the packaging and put aside. If the Pull-Through Tool disconnects from the conduit during loading, proceed as follows: ► Pull the Pull-Through Tool 5 from the Cartridge 3a. ► If the conduit can be grasped from the rear inlet opening of the cartridge: – Pull the end of the conduit completely out of the cartridge. Proceed carefully so that the conduit does not tear. – Compress the handle of the Pull-Through Tool 5 until it clicks in, so that the wire hooks 5b intermesh. – Insert Pull-Through Tool 5 carefully through the Implant end into the Cartridge 3a. When doing so, make certain that the Implant tines are not damaged. – Release the handle of the Pull-Through Tool 5 (press releaser 5a), lock securely in the shell and reattach Stop Clip 4. – Repeat the loading process. ► If the conduit cannot be removed by careful, continuous application of force or the conduit cannot be grasped from the rear inlet opening, disassemble the cartridge: – The long tube holding the Implant consists of a top and a bottom half, which can be separated in the longitudinal direction. They are fixed to the end the Implant sits on. Grasp the tube with one hand and the cartridge with the other and pull until the tube releases from the cartridge. – Open the top and bottom tube halves by releasing the retainers which hold the tube in the cartridge. – Remove conduit – Dispose of the PAS-Port Proximal Anastomosis System and repeat the loading process with a new PAS-Port Proximal Anastomosis System. If the conduit was accidentally pulled too far over the Implant, proceed as follows: ► Do not attempt to pull the conduit back into the Cartridge 3a because the Implant tines can be damaged when doing so. ► Pull conduit completely through the Cartridge 3a and remove. ► Remove the conduit from the Pull-Through Tool 5 and repeat the loading process.
► Use Vein/Aorta Gauge 6 to determine the suitability of the conduit:
2.5.6
– For the application, place provided end of the conduit in Conduit Outside Diameter Slots 6b of the Vein/Aorta Gauge – To estimate the doubled wall thickness of the conduit, place the conduit in Conduit Double Wall Thickness Slots 6c in the insufflated state. – Read the number on the smallest slot into which the conduit can easily be inserted or from which it can be easily pulled. – Do not use conduit vessels with an outside diameter of less than 4 mm or more than 6 mm with doubled wall thicknesses equaling more than 1.4 mm ► Ensure that the end of the conduit to be connected to the Implant has an area about 15 mm long without valves or lateral branches. ► Cleanly sever the conduit on the end intended for connection to the Implant at an angle of approx. 90°. Take note of the direction of flow through the conduit. ► Determine appropriate length for the conduit: – Use thread or suture material and mark the anticipated required length of the conduit with clips. – Adjust filled conduit to the length marked with thread or suture material.
► Grasp conduit with two fine tweezers at two points offset by 180° and carefully evert over the Anastomosing
Note The risk of kinking the Implant can be minimized if the correct conduit length is determined when the heart is contracting and filled with blood.
► Carefully retract Poke-Through Tool 2 in a straight line and remove, see Fig. H.
► Store conduit in an acellular physiological solution until use.
2.5.3
Preparing the target vessel
► Determine conduit placement:
– In the case of conduits that are destined for the left-lateral heart wall, the left-posterior or the left-anterior myocardium area, the anastomoses are placed on the concave left-lateral wall of the ascending target vessel or aortic arch. – In the case of conduits that are destined for the right-lateral or right-posterior heart surface, the anastomoses are placed on the anterior surface of the ascending target vessel and can be guided on the left, away over the right auricula, or along past it. – Placement of the PAS-Port Implant on the right-lateral wall of the ascending target vessel is to be avoided because there is greater risk for Implant kinks or external compression here. Place individual retaining seams along the course of the transplant as required in order to prevent buckling after closing the thorax. ► Use Target Vessel Slot 6a of the Vein/Aorta Gauge 6 in order to examine the suitability of the target vessel at the site of the planned proximal anastomosis: Do not use the PAS-Port Proximal Anastomosis System on target vessels with outside diameters of 18 mm or less. ► Palpate to ensure that the target vessel has a length of at least 25 mm without significant changes and/or disease. The area intended by the surgeon for placement of the proximal anastomosis should be of a quality sufficient for a hand-sutured anastomosis to also be considered. ► Perform a denudation of the intended anastomosis area only when excessively strong connective tissue is present.
2.5.4
Opening the packaging of the PAS-Port Proximal Anastomosis System
WARNING Risk to patient due to contamination! The inner shell and its cover are sterile. ► Handle the inner shell and its cover only while observing sterile precautionary measures. ► Open the packaging of the PAS-Port Proximal Anastomosis System and dispose of the outer packaging material. ► Remove and dispose of the cover of the inner shell. ► Leave all components of the system in their compartments in the inner shell.
Everting and puncturing conduit
Implant 3b so that all nine tines are covered (see Fig. C and D). When the conduit is everted properly, the intima is visible on the outer periphery of the Implant. The conduit may not be everted less than 2 mm and not more than 5 mm over the tines of the Implant. If the conduit cannot be everted without problems, it may not be used, even if it fulfills the specifications for use with the PAS-Port Proximal Anastomosis System. Note In order to inspect the eversion, it may be necessary to remove the Cartridge 3a by carefully releasing the holder from the inner shell. ► After inspecting the eversion, place the Cartridge 3a back in the holder of the inner shell. When doing so, ensure
that the components latch back into place in their respective positions. ► Remove one of the Poke-Through Tools 2 and, with the narrow end toward the Implant, lay in the groove of the
inner shell that aligns with the Cartridge 3a, see Fig. E. ► With one hand, press the gray tube of the cartridge in the inner shell slightly; with the other hand, advance the
Poke-Through Tool 2 up to the stop over the Anastomosing Implant 3b, see Fig. F and G. The conduit remains everted to the base of the Implant. ► If the Anastomosing Implant 3b was not pulled back: re-evert Implant with fine tweezers. When doing so, ensure
that the Implant is not damaged by this process. ► Ensure that all nine tines of the Anastomosing Implant 3b are symmetrical and not bent. In the case of a bent
tine, remove the conduit and dispose of the PAS-Port Proximal Anastomosis System: – Load Cartridge 3a into the Delivery Tool 1 and trigger Delivery Tool in the air in the sterile surgical area. – Pull conduit from the device with tweezers and place on a sterile surface. – Separate conduit from the Implant with a cut. – To remove the conduit, it can also be pulled back and pulled out of the cartridge. – Remove any conduit areas damaged by the tines. – Repeat the loading process with a new PAS-Port Proximal Anastomosis System. ► Fill the reservoir of the cartridge with acellular physiological solution in order to keep the conduit moist and viable until immediately before loading into the Delivery Tool.
2.5.7
Loading cartridge into Delivery Tool
WARNING Risk of injury! ► Do not touch sharp Auger Tip (bar drill) 1c on the Deployment End 1d. ► When the surgeon is ready to begin creating the proximal anastomosis, remove the Cartridge 3a from the inner
shell. ► Lay the Implant end of the Cartridge 3a on the Guide Clip 1a and advance cartridge until its base sits on the rails
of the Delivery Tool 1. When loading, carefully make certain not to damage the Implant. ► Remove Guide Clip 1a by pulling on the lug. ► Grasp the housing of the Delivery Tool 1 securely with one hand and advance the Cartridge 3a with the other
until it latches. The Cartridge 3a is completely inserted when it audibly clicks and the Knob 1g partially turns. This step is irreversible. The PAS-Port Proximal Anastomosis System is now ready for use.
2.5.8
Attaching the Implant
Note The risk of buckling the transplant can be minimized by careful selection of the anastomosis site on the target vessel, see Preparing the target vessel. ► Prepare the target vessel at the intended anastomosis site by briefly cauterizing the connective tissue on the
adventitia in a circular area of approx. 4 mm in diameter. ► Remove Delivery Tool 1 from the inner shell and slide the Safety Switch 1f into the unlocked position to unlock,
see Fig. I.
WARNING Danger of injury due to premature activation of the cutter! As soon as the Safety Switch 1f is in the unlocked position, turning the Knob 1g causes immediate activation of the cutter. ► Do not unlock Safety Switch 1f until the conduit is to be applied. Note If the Cartridge 3a is incorrectly loaded in the Delivery Tool 1, the Safety Switch 1f cannot be unlocked. ► Position Delivery Tool 1 at the prepared anastomosis site at a right angle to the surface of the target vessel. ► Puncture target vessel with the Auger Tip 1c.
If the Auger Tip cannot easily puncture the target vessel: choose another anastomosis site. ► Ensure that there is full-surface contact between the Delivery Tool 1 and the surface of the target vessel, without
the target vessel being compressed or incised. After placement on the target vessel, do not move the Delivery Tool 1 laterally and do not hold in the air over the target vessel. ► Align the Delivery Tool 1 so that a visual inspection of the attaching process is possible through the Opening 1e for surgical setting. ► Ensure that the average arterial pressure equals at least 50 mmHg when attaching. ► To complete the anastomosis: – Rotate the Knob 1g clockwise up to the perceptible stop. – There is an arrow on the Knob 1g which points at the rearward inlet opening of the cartridge after one full Knob rotation, see Fig. J. – Ensure that the Auger Tip 1c has contact with the surface of the target vessel during the entire attachment process and that the target vessel is neither compressed nor incised by the Delivery Tool 1. After completing the aortotomy, blood can flow unhindered through the Seal Housing 1b into the surgical site before insertion of the Implant in the target vessel. ► Keep surgical site clear with a suction instrument as required. ► If blood flow into the Seal Housing 1b fails to appear or flows only slowly: abort attachment and repair the target vessel with routine surgical techniques as required, see Corrective measures in case of problems. ► After reaching the stop of Knob 1g: – Grasp conduit with tweezers tightly on the Implant and slowly raise the Delivery Tool 1 from the target vessel – Grasping the conduit near the Implant when removing the device avoids tensile stress on the anastomosis and enables the collapsing of theconduit. This causes a diameter reduction in the case of a vessel filled with blood. – When grasping the conduit, avoid manipulating the tines on the Delivery Tool 1, because they can be released from the Delivery Tool. WARNING Risk to patient from post-operative bleeding! ► Stabilize conduit with tweezers before removing the Delivery Tool.
Only process chemicals that have been tested and approved (e.g. VAH or FDA approval or CE mark) and which are compatible with the product’s materials according to the chemical manufacturers’ recommendations may be used for processing the product. All the chemical manufacturer's application specifications must be strictly observed. Failure to do so can result in the following problems: ■ Optical changes of materials, e.g. fading or discoloration of titanium or aluminum. For aluminum, the application/process solution only needs to be of pH >8 to cause visible surface changes. ■ Material damage such as corrosion, cracks, fracturing, premature aging or swelling. ► Do not use metal cleaning brushes or other abrasives that would damage the product surfaces and could cause corrosion. ► Further detailed advice on hygienically safe and material-/value-preserving reprocessing can be found at www.a-k-i.org, link to "AKI-Brochures", "Red brochure".
3.3
Single-use products
Art. no.
Designation
FC700SU
PAS-Port Proximal Anastomosis System
► Do not reuse the product.
The reprocessing of the product affects its functionality. Risk of injury, illness or death due to soiling and/or impaired functionality of the product. ► Do not reprocess the product.
3.4
Limitations on reuse
Art. no.
Designation
FC705
Vein/Aorta Gauge
■ The product can be used up to 12 times with the proper care and if it is undamaged and clean. Any additional reuse falls under the responsibility of the user.
■ The life of the product is limited by damage, normal wear and tear, type and duration of use, as well as handling, storage and transport of the product.
■ A careful visual and functional inspection before the next use is the best opportunity to recognize a product that is no longer functional.
3.5
Preparations at the place of use
► If applicable, rinse non-visible surfaces preferably with deionized water, with a disposable syringe for example. ► Remove any visible surgical residues to the extent possible with a damp, lint-free cloth. ► Transport the dry product in a sealed waste container for cleaning and disinfection within 6 hours.
3.6
Cleaning/Disinfection
the device by flushing an acellular physiological solution via the inlet opening on the Knob End 1g of the Delivery Tool 1. ► If no hemostasis is apparent, see Corrective measures in case of problems. ► Remove Delivery Tool 1 from the surgical site and check whether all of the other 9 tines are present. ► Using routine surgical technique, set a suitable clip on the end of the Implant. ► Before closing the thorax, proceed as follows: – Examine anastomosis for leaks and ensure that the transplant appears to have been attached correctly. – After placing the proximal and distal anastomosis, check the strain effect on the transplant with the heart filled with blood and in normal position. – Check transplant for blood flow. – In the case of anastomosis leaks, see Corrective measures in case of problems.
3.6.1
Product-specific safety information on the reprocessing method
WARNING Risk to patient from post-operative bleeding! ► Examine anastomosis after completion.
3.6.2
► If the conduit dries on the inner side of the Delivery Tool 1 and is difficult to remove: moisten the conduit and
► If the Implant was attached incompletely or incorrectly (individual tines of the outer Implant flange do not con-
tact the adventitia and therefore do not have complete contact to the connective tissue of the target vessel), or if the Implant is not seated securely: – Remove the Implant, see Corrective measures in case of problems. – Do not manipulate tines. ► Place individual retaining seams along the course of the transplant as required in order to prevent buckling. ► If there is no blood flow through the transplant, see Corrective measures in case of problems.
2.5.9
Corrective measures in case of problems
► If there is an anastomosis bleed after attaching the Implant, the surgeon can attempt to achieve hemostasis with
a pouch-string suture around the Implant. If hemostasis cannot be achieved, observe the following step. ► If there is no blood flow into the Seal Housing during attachment of the device, no hemostasis, no blood flow into the transplant after attachment of the device or in the case of incorrect attachment of the device: – Set a curved vessel clip around the Implant. – Press the Implant body toward the center of the Implant with a needle holder and remove. – Repair originally intended anastomosis site.
3.
Validated reprocessing procedure
3.1
General safety information
Note Adhere to national statutory regulations, national and international standards and directives, and local, clinical hygiene instructions for sterile processing.
Damage to or destruction of the product due to inappropriate cleaning/disinfecting agents and/or excessive temperatures! ► Following the manufacturer's instructions, use cleaning and disinfecting agents – that are approved for plastic materials. – that do not attack softeners (e.g., in silicone). ► Observe specifications regarding concentration, temperature and exposure time. ► Do not exceed the maximum allowable disinfection temperature of 93 °C. ► Use suitable cleaning/disinfecting agents if the product is put away in a wet condition. To prevent foaming and
degradation of the efficacy of the process chemicals: prior to mechanical cleaning and disinfection, rinse the product thoroughly with running water
Validated cleaning and disinfection procedure
Validated procedure
Specific requirements
Reference
Manual cleaning with immersion disinfection
■ Suitable cleaning brush ■ Single use syringe 20 ml ■ Drying phase: Use a lint-free
Chapter Manual cleaning/disinfection and subsection:
■ Vein/Aorta Gauge FC705
■ Chapter Manual cleaning with immersion disinfection
cloth or medical compressed air Mechanical alkaline cleaning and thermal disinfection
■ Place the product on a tray that
■ Vein/Aorta Gauge FC705
is suitable for cleaning (avoid rinsing blind spots).
Chapter Mechanical cleaning/disinfection and subsection:
■ Chapter Mechanical alkaline cleaning and thermal disinfection
3.7
Manual cleaning/disinfection
3.7.1
Manual cleaning with immersion disinfection
Phase
Step
T [°C/°F]
t [min]
Conc. [%]
Water quality
Chemical
I
Disinfecting cleaning
RT (cold)
>15
2
D–W
Aldehyde-free, phenol-free, and QUAT-free concentrate, pH ~ 9*
II
Intermediate rinse
RT (cold)
1
-
D–W
-
Note For patients with Creutzfeldt-Jakob disease (CJD), suspected CJD or possible variants of CJD, observe the relevant national regulations concerning the reprocessing of products.
III
Disinfection
RT (cold)
5
2
D–W
Aldehyde-free, phenol-free, and QUAT-free concentrate, pH ~ 9*
Note Mechanical reprocessing should be favored over manual cleaning as it gives better and more reliable results.
IV
Final rinse
RT (cold)
1
-
FD-W
-
Note Successful processing of this medical device can only be ensured if the processing method is first validated. The operator/sterile processing technician is responsible for this.
V
Drying
RT
-
-
-
-
Note If there is no final sterilization, then a virucidal disinfectant must be used.
D–W: FD–W:
Note For up-to-date information about reprocessing and material compatibility, see B. Braun eIFU at eifu.bbraun.com The validated steam sterilization procedure was carried out in the Aesculap sterile container system.
3.2
General information
Dried or affixed surgical residues can make cleaning more difficult or ineffective and lead to corrosion. Therefore the time interval between application and processing should not exceed 6 h; also, neither fixating pre-cleaning temperatures >45 °C nor fixating disinfecting agents (active ingredient: aldehydes/alcohols) should be used. Excessive measures of neutralizing agents or basic cleaners may result in a chemical attack and/or to fading and the laser marking becoming unreadable visually or by machine for stainless steel. Residues containing chlorine or chlorides e.g. in surgical residues, medicines, saline solutions and in the service water used for cleaning, disinfection and sterilization will cause corrosion damage (pitting, stress corrosion) and result in the destruction of stainless steel products. These must be removed by rinsing thoroughly with demineralized water and then drying. Additional drying, if necessary.
Drinking water Fully desalinated water (demineralized, low microbiological contamination: drinking water quality at least) RT: Room temperature *Recommended: BBraun Stabimed fresh ► Note the information on appropriate cleaning brushes and disposable syringes, see Validated cleaning and dis-
infection procedure. Phase I ► Fully immerse the product in the cleaning/disinfectant for at least 15 min. Ensure that all accessible surfaces are moistened. ► Clean the product with a suitable cleaning brush in the solution until all discernible residues have been removed from the surface. ► If applicable, brush through non-visible surfaces with an appropriate cleaning brush for at least 1 min. ► Mobilize non-rigid components, such as set screws, links, etc. during cleaning. ► Thoroughly rinse through these components with the cleaning disinfectant solution (at least five times), using a disposable syringe.
Phase II ► Rinse/flush the product thoroughly (all accessible surfaces) under running water. ► Mobilize non-rigid components, such as set screws, joints, etc. during rinsing. ► Drain any remaining water fully. Phase III ► Fully immerse the product in the disinfectant solution. ► Mobilize non-rigid components, such as set screws, joints, etc. during rinsing. ► Rinse lumens at least 5 times at the beginning of the exposure time using an appropriate disposable syringe. Ensure that all accessible surfaces are moistened. Phase IV ► Rinse/flush the product thoroughly (all accessible surfaces). ► Mobilize non-rigid components, such as set screws, joints, etc. during final rinse. ► Rinse lumens with an appropriate disposable syringe at least five times. ► Drain any remaining water fully. Phase V ► Dry the product in the drying phase with suitable equipment (e.g. cloth, compressed air), see Validated cleaning and disinfection procedure.
3.8
5.
Technical service
CAUTION Modifications carried out on medical technical equipment may result in loss of guarantee/warranty rights and forfeiture of applicable licenses. ► Do not modify the product. ► For service and repairs, please contact your national B. Braun/Aesculap agency. Service addresses Aesculap Technischer Service Am Aesculap-Platz 78532 Tuttlingen / Germany Phone: +49 7461 95-1601 Fax: +49 7461 16-2887 E-Mail: [email protected] Other service addresses can be obtained from the address indicated above.
6.
Disposal
► Adhere to national regulations when disposing of or recycling the product, its components and its packaging.
Mechanical cleaning/disinfection
Note The cleaning and disinfection device must be of tested and approved effectiveness (e.g. FDA approval or CE mark according to DIN EN ISO 15883).
7.
Symbols on product and packaging Caution Observe important safety information such as warnings and precautions in the instructions for use.
Note The cleaning and disinfection device used for processing must be serviced and checked at regular intervals.
3.8.1
Mechanical alkaline cleaning and thermal disinfection
Follow the instructions for use
Machine type: single-chamber cleaning/disinfection device without ultrasound Phase
Step
T [°C/°F]
t [min]
Water quality
Chemical/Note
I
Pre-rinse
<25/77
3
D–W
-
II
Cleaning
55/131
10
FD-W
■ Concentrate, alkaline:
Sterilization using irradiation Non-sterile medical product
– pH = 13 – <5 % anionic surfactant
■ 0.5 % working solution – pH = 11* III
Intermediate rinse
>10/50
1
FD-W
-
IV
Thermal disinfecting
90/194
5
FD-W
-
V
Drying
-
-
-
According to the program for cleaning and disinfection device
Not for reuse in intended applications as defined by the manufacturer
Use by
D–W: FD–W:
Drinking water Fully desalinated water (demineralized, low microbiological contamination: drinking water quality at least) *Recommended: BBraun Helimatic Cleaner alcaline
Manufacturer combined with date of manufacture (year)
► Check visible surfaces for residues after mechanical cleaning/disinfecting.
3.9
Inspection
Date of manufacture
► Allow the product to cool down to room temperature. ► Dry the product if it is wet or damp.
3.9.1
Visual inspection
► Ensure that all contamination has been removed. In particular, pay attention to recessed areas. ► If the product is dirty: repeat the cleaning and disinfection process. ► Check the product for damage, e.g. loose, bent, broken, cracked, worn or severely scratched and fractured com-
SN
Manufacturer’s serial number
► Check the product for missing or faded labels. ► Check the surfaces for rough spots. ► Set aside the product if it is damaged.
LOT
Manufacturer’s batch designation
3.9.2
REF
Manufacturer’s article number
QTY
Delivery quantity
ponents.
Functional test
► Check for compatibility with associated products. ► Immediately put aside inoperative products and send them to Aesculap Technical Service, see Technical service.
3.10 Packaging ► Place the product in its holder or on a suitable tray. Ensure that sharp edges are covered. ► Package trays appropriately for the sterilization process (e.g. in Aesculap sterile containers). ► Ensure that the packaging provides sufficient protection against contamination of the product during storage.
CE-approved in accordance with Directive 93/42/EEC
3.11 Steam sterilization Keep device away from fluids
► Check to ensure that the sterilizing agent will come into contact with all external and internal surfaces (e.g., by
opening any valves and faucets). ► Validated sterilization process – Steam sterilization using fractional vacuum process – Steam sterilizer according to DIN EN 285 and validated according to DIN EN ISO 17665 – Sterilization using fractionated vacuum process at 134 °C/holding time 5 min ► If several devices are sterilized at the same time in the same steam sterilizer: Ensure that the maximum permitted load according to the manufacturers’ specifications is not exceeded.
4.
Conditionally MR compatible
Storage
► Store sterile products in germ-proof packaging, protected from dust, in a dry, dark, temperature-controlled area. ► Store sterile single-use products in germ-proof packaging in a dust-protected, dry, dark and temperature-con-
trolled room.
4.1
Ambient conditions
The following environmental conditions apply to the transport and storage of the product: Temperature
-10 °C to 50 °C
Relative humidity
10 % to 90 %
Atmospheric pressure
500 hPa to 1 060 hPa
TA015510
2020-05
V6
Change No. 63066