Quick Tips
8 Pages
Preview
Page 1
AVEA ventilator quick tips ®
Critical care ventilation
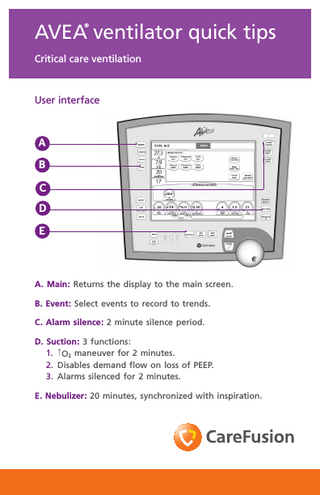
User interface
A B C D E
A. Main: Returns the display to the main screen. B. Event: Select events to record to trends. C. Alarm silence: 2 minute silence period. D. Suction: 3 functions: 1. ↑O2 maneuver for 2 minutes. 2. Disables demand flow on loss of PEEP. 3. Alarms silenced for 2 minutes. E. Nebulizer: 20 minutes, synchronized with inspiration.
®
The AVEA ventilator’s quick tips card is not intended as a replacement for the operator’s manual. You must become completely familiar with the operator’s manual before using the AVEA ventilator.
Touch-Turn-Touch™ and Touch-Turn-Accept™ method 1. Touch the control to select. The control changes color indicating that it is active.
1
2. Turn the data dial to reach the selected value. 3. Touch the control again or press ACCEPT to confirm the change.
2
3
Setting alarm limits 1. Press the ALARM LIMITS button to open or close the window. 2. Use Touch-Turn-Touch or Touch-Turn-Accept method to modify alarms.
1
2
Proximal flow sensors The AVEA ventilator accepts either hot wire or variable orifice proximal low sensors. These are in addition to the internal inspiratory flow sensor and heated expiratory flow sensor. The variable orifice sensor attaches to the receptacle circled in dark blue. The hot wire flow sensor attaches to the receptacle circled in light blue directly below the variable orifice flow sensor connection. To attach, pull back the locking collar. Push firmly onto the receptacle. Push the collar forward to lock the sensor in place. To disconnect, retract the collar and pull the connector straight away from the ventilator.
Monitors and definitions Volume monitors Vte
Exhaled tidal volume.
Vte/kg
Exhaled tidal volume adjusted for patient weight.
Vti
Inspired tidal volume.
Vti/kg
Inspired tidal volume adjusted for patient weight.
Spon Vt
Spontaneous tidal volume.
Spon Vt/kg
Spontaneous tidal volume adjusted for patient weight.
Mand Vt
Mandatory tidal volume: Displayed as a rolling average of either 8 breaths or one minute, whichever occurs first.
Mand Vt/kg
Mandatory tidal volume adjusted for patient weight.
Vdel % leak Ve
Delivered machine volume measured by the ventilator’s inspiratory flow sensor. Percent leakage: The difference between the inspired and exhaled tidal volumes in terms of % difference. Minute volume. Volume of gas exhaled by the patient during the last minute.
Ve/kg
Minute volume adjusted for patient weight.
Spon Ve
Spontaneous minute volume.
Spon Ve/kg
Spontaneous minute volume adjusted for patient weight.
Rate/time monitors Rate
Breath rate.
Spon rate
Spontaneous breath rate.
Ti
Inspiratory time.
Te
Exhalation time.
I:E
Inspiratory/expiratory ratio. Note: Not active for demand breaths.
f/Vt
Rapid shallow breathing index.
Pressure monitors Ppeak
Peak inspiratory pressure. Note: Not active with spontaneous breaths.
Pmean
Mean airway pressure.
Pplat
Plateau pressure. If no plateau occurs, then the monitor displays.***
PEEP
Positive end expiratory pressure.
Air inlet
Air inlet gas supply pressure.
O2 inlet
Oxygen inlet gas supply pressure.
Gas composition monitors FiO2
Delivered percent O2 .
Mechanics CDYN CDYN/Kg
Dynamic compliance (CDYN and CDYN/Kg), absolute and normalized to patient weight.
Monitors and definitions (continued) Mechanics (continued)
PIFR
Respiratory system compliance (C RS ), (a.k.a. static compliance Cstat), absolute and normalized to patient weight. Note: This requires an Inspiratory Hold maneuver. Peak inspiratory flow rate.
PEFR
Peak expiratory flow rate.
Ccw
The ratio of the tidal volume (exhaled) to the delta esophageal Pressure (dPES ). Requires an esophageal balloon.
Cstat Cstat/kg
CLUNG
C 20 / C
R RS
R PEAK R IMP
R LUNG
The ratio of the tidal volume (exhaled) to the delta transpulmonary pressure. The delta transpulmonary pressure is the difference between the airway plateau pressure (during an inspiratory pause) and esophageal pressure (at the time the airway plateau pressure is measured) minus the difference between the airway and esophageal baseline pressures. Requires an inspiratory hold and esophageal balloon. The ratio of the dynamic compliance during the last 20% of inspiration (C 20 ) to the total dynamic compliance (C). The total resistance during the inspiratory phase of a breath. Respiratory system resistance is the ratio of the airway pressure differential (peak–plateau) to the inspiratory flow 12 ms prior to the end of inspiration. Requires an inspiratory hold. The peak expiratory resistance (R PEAK ) is defined as the resistance at the time of the peak expiratory flow (PEFR). The airway resistance between the wye of the patient circuit and the tracheal sensor. Requires an inspiratory hold and tracheal catheter. The ratio of the tracheal pressure differential (peak–plateau) to the inspiratory flow 12 ms prior to the end of inspiration. Requires an inspiratory hold and tracheal catheter.
dPAW
The difference between peak airway pressure (P PEAK AW ) and baseline airway pressure (PEEPAW ).
dPES
The difference between peak esophageal pressure (PPEAK ES ) and baseline esophageal pressure (PEEPES ).
AutoPEEP
dAutoPEEP
The airway pressure at the end of an expiratory hold maneuver. Requires a passive patient. The difference between airway pressure at the end of an expiratory hold maneuver and the airway pressure at the start of the next scheduled breath after the expiratory hold maneuver. Requires a passive patient.
AutoPEEPES
The difference between esophageal pressure measured at the end of exhalation (PEEPES ) minus the esophageal pressure measured at the start of a patient-initiated breath (PES start ) and the sensitivity of the ventilator’s demand system. The sensitivity of the ventilator’s demand system is the difference between the baseline airway pressure (PEEPAW ) and the airway pressure when the patient initiates a breath (PAW start). Requires an esophageal balloon.
Ptp Plat
Transpulmonary pressure during an inspiratory hold, which is the difference between the airway plateau pressure (PPLAT AW ) and the corresponding esophageal pressure. Requires an inspiratory hold and esophageal balloon.
Monitors and definitions (continued) Mechanics (continued) Ptp PEEP
MIP P100
WOBV
WOB P
WOB I
The difference between the corresponding airway and esophageal pressures at the end of the expiratory hold during an AutoPEEP maneuver. Requires an inspiratory hold and esophageal catheter. The maximum negative airway pressure that is achieved by the patient, during an expiratory hold maneuver. The negative pressure that occurs 100 ms after an inspiratory effort has been detected. Ventilator work of breathing (WOBV ) is defined as the summation of airway pressure (PAW) minus the baseline airway pressure (PEEPAW) times the change in tidal volume to the patient (-V) during inspiration, and normalized to the total inspiratory tidal volume (Vti). Patient work of breathing (WOB P ), normalized to the total inspiratory tidal volume. Patient work of breathing is defined as the summation of two work components: Work of the lung and work of the chest wall. Requires an esophageal balloon. Imposed work of breathing (WOBI) is defined as the work performed by the patient to breathe spontaneously through the breathing apparatus, (i.e., the E.T. tube), the breathing circuit and the demand flow system. Requires a tracheal catheter. Note: Monitored values are displayed as BTPS.
Capnography EtCO2
VCO2
VtCO2
Vd ana
Vd/Vt ana
Vd phy Vd/Vt phy
Vd alv
The patient’s peak expired CO2 as measured and reported by the CO2 sensor in the airway, calculated for each breath then averaged as specified by set EtCO2 averaging time. Minute volume of exhaled CO2 measured continuously and averaged over a user-selectable time. Requires flow measurement at the wye or circuit compliance active. Tidal volume of exhaled CO2 , measured for each breath and then averaged over the set VCO2 averaging time. Requires flow measurement at the wye or circuit compliance active. The volume of dead space in the patient’s conducting airways from the nose to the level of the terminal bronchioles measured for each breath, then averaged over the set CO2 averaging time. Also includes any mechanical dead spaces added to the ventilator circuit between the CO2 sensor and the patient. Requires flow measurement at the wye or circuit compliance active. Anatomic Vd/Vt is averaged over the set VCO2 averaging time. Requires flow measurement at the wye or circuit compliance active. Comprises Vd ana as well as the volume of the respiratory zone (respiratory bronchioles, alveolar ducts and alveoli) not participating in gas exchange. Requires an arterial blood gas sample. Physiologic Vd/Vt is averaged over the set VCO2 averaging time. Requires an arterial blood gas sample. Alveolar dead space is the difference between physiological dead space and anatomical dead space. It represents the volume of the respiratory zone that is from ventilation of relative under-perfused or non-perfused alveoli. Requires an arterial blood gas sample.
Monitors and definitions (continued) Capnography (continued) VA
Alveolar ventilation is the volume of gas participating in gas exchange per minute. Requires an arterial blood gas sample.
P/F
The PaO2 / FIO2 ratio is a simple assessment of gas exchange calculated from the FIO2 monitor value and an arterial blood oxygen measurement (required) entered by the clinician.
OI
Oxygenation index is a dimensionless number often used to assess the “pressure cost” of oxygenation calculated from the FIO2 mean airway pressure and an arterial blood oxygen measurement (required) entered by the clinician.
Available modes Mode
Adult
Pediatric
Neonatal
Volume A/C
X
X
X
Volume SIMV
X
X
X
Pressure A/C*
X
X
X
Pressure SIMV*
X
X
X
TCPL A/C*
X
TCPL SIMV*
X
PRVC A/C
X
X
PRVC SIMV
X
X
APRV/BiPhasic
X
X
CPAP/ PSV
X
X
Nasal CPAP/IMV
* Volume guarantee breaths available for neonates
X
Normal values and indications for weaning (adults) Parameter
Normal range
Indications for weaning
Respiratory rate
10 to 20 breaths/minute
< 30 B/min△
Esophageal pressure
5 to 10 cmH2O
< 15 cmH2O
Tidal volume
7 to 10 mL/kg
> 5 mL/kg△
Minute ventilation
5 to 10 Liters/min
< 10 L/min
WOB P
3 to 0.6 Joules/Liter
< 0.75 J/L △
Pressure time index
0.05 to 0.12
< 0.15 △
Airway resistance
2 to 5 cmH2O/L/s
< 15 cmH2O/L/s
Lung compliance
50 to 100 mL/cmH2O
> 25 mL/cmH2O
Maximum inspiratory
-30 cmH2O low effort
> -20 cmH2O△
Pressure (MIP)
-140 cmH2O high effort
Auto PEEP
0
< 3 cmH2O
Respiratory drive P0.1
2 to 4 cmH2O
< 6 cmH2O△
f/VT
60 to 90
< 105
Pressure time
200 to 300 cmH2O sec/min
Product (PTP) Ti/TTOT
0.3 to 0.4
Parameter
Acceptable range
SaO2
> 90% on FlO2 of < 40%
P(A - a) O2 on FlO2 of 100%
< 350 mmHg
PaO2 /FlO2
> 200 mmHg
Qs/Qt
< 20%
Vd/Vt
< 0.6
Heart rate
> 70 and < 120 bpm
Mean blood pressure
> 70 and < 110 mmHg
Note: Research indicates these pulmonary parameters may aid qualified medical personnel in evaluating weaning potential. If measured values exceed acceptable range, successful weaning may be less likely. Ranges from these parameters are not intended as a substitute for clinical assessment by qualified medical personnel and CareFusion assumes no liability for their use in patient care. A list of references is available upon request.
© 2011 CareFusion Corporation or one of its subsidiaries. All rights reserved. AVEA, Touch-Turn-Accept and TouchTurn-Touch are trademarks or registered trademarks of CareFusion Corporation or one of its subsidiaries. RC2236 (0511/2000) L3059 Rev. B
CareFusion 22745 Savi Ranch Parkway Yorba Linda, CA 92887 800.231.2466 toll-free 714.283.2228 tel 714.283.8493 fax
CareFusion Yorba Linda, CA
carefusion.com
CareFusion Germany 234 GmbH Leibnizstrasse 7 97204 Hoechberg Germany +49 931 4972-0 tel +49 931 4972-423 fax