Parks Medical
Model 811-B and 811-BTS Instruction Manual Oct 2003
Instruction Manual
28 Pages
Preview
Page 1
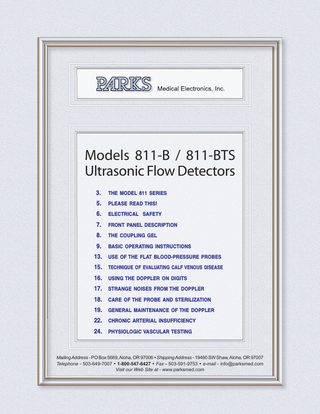
Models 811-B / 811-BTS Ultrasonic Flow Detectors 3.
THE MODEL 811 SERIES
5.
PLEASE READ THIS!
6.
ELECTRICAL SAFETY
7.
FRONT PANEL DESCRIPTION
8.
THE COUPLING GEL
9.
BASIC OPERATING INSTRUCTIONS
13. USE OF THE FLAT BLOOD-PRESSURE PROBES 15. TECHNIQUE OF EVALUATING CALF VENOUS DISEASE 16. USING THE DOPPLER ON DIGITS 17. STRANGE NOISES FROM THE DOPPLER 18. CARE OF THE PROBE AND STERILIZATION 19. GENERAL MAINTENANCE OF THE DOPPLER 22. CHRONIC ARTERIAL INSUFFICIENCY 24. PHYSIOLOGIC VASCULAR TESTING
Mailing Address - PO Box 5669, Aloha, OR 97006 Shipping Address - 19460 SW Shaw, Aloha, OR 97007 Telephone - 503-649-7007 1-800-547-6427 Fax - 503-591-9753 e-mail - [email protected] Visit our Web Site at - www.parksmed.com
Parks Medical Electronics, Inc. Models 811-B and 811-BTS
2
Medical Electronics, Inc.
THE MODEL 811 SERIES Ultrasonic Doppler Flow Detector PEDIATRICS SURGICAL WARD INTENSIVE CARE RECOVERY ROOM The Model 811 and its variations have been our most popular instruments for over twenty years. They have been internally modified over that period to keep abreast of newer technology, but the “black box” package remains the same. We now offer this basic design in a variety of housings, some of which are shown in this leaflet. Other cases with removable lids which can also store cuffs, manometer and gel are available at additional cost. All Model 811 series Dopplers are made in operating frequencies from 8 to 9.7 MHz. If you already have PARKS instruments with detachable probes in your hospital or office, we suggest you purchase the same frequency Doppler in one of these styles so your probes will be interchangeable.
How Systolic Pressure Measurements are Made Essentially, the Doppler substitutes for a stethoscope when a stethoscope won’t work or results are of doubtful accuracy. An ordinary blood-pressure cuff is used above the elbow. The flat Doppler probe (with contact gel applied) is placed over the radial artery before the cuff is inflated and its position is optimized to give the loudest flow signal (a pulsing, hissing noise). The cuff is inflated rapidly to above systolic pressure and then gradually deflated. As cuff pressure falls to systolic pressure, a pulsing flow sound is heard during a very short portion of the cardiac cycle. At that moment the manometer reading is equivalent to systolic pressure. As pressure falls further, the dicrotic notch may be heard in the flow sound, allowing you to estimate diastolic pressure. We make no claim as to the accuracy of the diastolic measurement because doctors use different subjective criteria. However, when
Model 811-B shown in standard aluminum box
systolic pressure is so low your stethoscope isn’t dependable, you’ll probably be quite satisfied with an accurate systolic measurement. Pressures as low as 10 mm Hg can be measured on premature infants. The accuracy of the determination depends on having the proper size cuff for the limb. Four probe styles are available, three of which are shown above. Flat probes are normally used for arm blood pressures but can be attached over the dorsalis pedis for post surgical determination of ankle blood pressures. The infant flat, adult flat and standard pencil probes are shown. A “skinny” pencil probe (1/4” diameter) is available for specialized applications. All probes can be gas sterilized but not autoclaved. Temperatures above 140 degrees Fahrenheit can ruin the probes. Our probes can be dropped without damage and are much less expensive to replace than those of competitive instruments. We advise having an extra probe on hand since the most likely cause of failure is the probe and / or its cable or connectors. These instruments don’t wear out. Many hundreds have been in service ten to twenty years. Probe and battery replacement will be necessary at some time, but can be ordered separately and installed by the user.
Model 811-B, the instrument shown on the front of this leaflet, will be the instrument of choice for most applications. It is shown housed in the standard welded aluminum box with no lid. It will not break, even if dropped. The interior is also impact resistant. A flashing light indicates the need for recharging the battery, but there is enough capacity for many blood pressure measurements or exams even when that point is reached. The instrument is designed to be left on charge when not in use.
Model 811-BL is for use in surgery when a
cautery is used. It has the same features as the 811-B plus a cautery suppressor with a controllable threshold that turns the sound off when the cautery noise gets too high. If you will not be using the Doppler while using a cautery, we recommend the Model 811-B or Model 811-BTS.
Model 811-BTS is our most reliable unit. Shown at the right in an aluminum carrying case with a removable lid and space for probes, gel and charger. It is normally supplied in the same aluminum box as the Model 811-B photo (extra charge for case shown at right). It was made for hospitals that check out Dopplers from Central Supply. The reason it is so reliable, besides the metal box, is that it cannot be left turned on inadvertently. When you push the on/off button the Doppler goes on for five minutes maximum. To shut it off, turn it on or extend the time, you simply push the button. The combination of a heavy-duty, long-life battery that can’t be overcharged, a metal box and structure that won’t break when dropped accidentally, and a timing circuit that prevents the unit from being left turned on combine to make this the instrument of choice for services where several people use the Doppler. An output for an amplifier or headphones (not included) means you can use it in ambulances and helicopters.
Model 811-BTS shown in Model 800 case Existing units originally sold in plastic boxes (Models 811, 812) and now in service can be put into either of the cases shown. Metal boxes are available in white, blue and black to show which hospital service the instrument belongs to.
Warranty
We warranty the 811 series Doppler against defects in materials and workmanship for one year. The warranty period on accessories and probes is six months. All warranty service is performed at the factory and all items must be returned to the factory prepaid. Specifically excluded from this warranty are any items which show evidence of physical abuse.
Thirty-Day Trial
We invite you to compare this Doppler with any other Doppler, regardless of price. A demonstration model is available to doctors and hospitals for a thirty-day trial. Trials are limited to the U.S.A. because of customs expense.
Ordering Information
All shipments are FOB Aloha, Oregon, shipping prepaid and added. Payment terms are net thirty days. For further information call us Toll-Free. Our office hours are 7:00 A.M. to 3:30 P.M. Pacific time.
Manufactured in the U.S.A. by:
PARKS Medical Electronics, Inc. 19460 S.W. Shaw, Aloha OR 97007
1-800-547-6427 or 503-649-7007 Fax 503-591-9753
Visit our Web Site at www.parksmed.com 3/18/03
Before You Begin, Please Read This!
Information contained in this operating manual is provided to help the user operate the instrument controls. In no way must a diagnosis be made on the basis of information provided in the manual. We provide generalized examples of waveforms and procedures which we believe to be in current usage. However, the procedure to be used and the diagnosis of an individual patient must be determined by the attending physician from information in scientific literature and from other medical sources.
114-0028-02
8/22/03
Parks Medical Electronics, Inc. Models 811-B and 811-BTS
5
Electrical Safety
CAUTION!!! Misuse of this equipment and inappropriate electrical connections will create a shock hazard. What appears to be simple connections to other equipment can put the patient and / or the operator at risk of electrical shock. FOLLOW THE MANUAL INSTRUCTIONS ON THE USE OF THIS EQUIPMENT. Avoid use involving electrical contact with other equipment. We assume no responsibility for misuse of our equipment. The following is a guide to avoiding common potential hazards, this is NOT comprehensive, always seek the advice of a qualified bioengineer BEFORE making any electrical connections. 1. CONNECTING TO A COMPUTER: Computers connected to our equipment without proper isolation from the power line are extremely hazardous. They must be battery operated with the charger disconnected, be operated from a medical grade power-line isolation transformer, or operated through optical isolators. Computer connections are potentially very hazardous. Your bioengineering department should review and approve of any proposed computer connections. 2. CONNECTING TO A POWER SUPPLY: Power supplies bought or built from “off-the-shelf” components may not provide isolation to medical standards. The safest way is to use medical grade isolation. Hospital bioengineering departments should be aware of the requirements and should be consulted prior to making power supply connections. 3. CONNECTING TO AN AMPLIFIER OR INTERCOM SYSTEM: A medical-grade isolation transformer or completely isolated battery operation is the safest means of connecting amplifiers or intercom systems. Helicopter services should have a qualified technician or bioengineer review all proposed connections. 4. OPERATING THIS EQUIPMENT WHILE ITS CHARGER IS PLUGGED INTO A POWER OUTLET IS A SHOCK HAZARD UNLESS A MEDICAL GRADE POWER ISOLATION TRANSFORMER IS USED. 5. OPERATION IN THE PRESENCE OF FLAMMABLE MATERIALS OR HIGH OXYGEN CONCENTRATIONS: The possibility of explosion or fire always exists when this equipment is used in such an environment. 6. PATIENT BURNS: These may occur through the probe when the Doppler is grounded (perhaps through an I.V. pole) and the electrocautery backplate has inadvertently not been connected. To protect against this ensure the cautery ground plate is on and only suspend the Doppler with an insulator.
SAFETY IS YOUR RESPONSIBILITY. IF IN DOUBT, SEEK EXPERT ADVICE. 107-0009-01
7/97
Parks Medical Electronics, Inc. Models 811-B and 811-BTS
6
Front Panel Description Models 811-B and 811-BTS The automatic shut off feature is the only functional difference between the PARKS Model 811-B and 811-BTS.
MODEL 811-B ONLY ON/OFF: This switch manually turns the Model 811-B on and off. POWER: This light will illuminate when the Model 811-B is turned on. The light will blink if the battery needs recharging. The instrument should be recharged as soon as possible after the light first begins to blink. However, the instrument will operate for about another hour after the light indicates charging is needed. We recommend you keep this unit on charge when it is not in use. You will get longer, more reliable service from the battery.
MODEL 811-BTS ONLY PUSH ON/OFF: The Model 811-BTS will be turned on and the push button will illuminate when momentarily depressed. The instrument may be turned off by again momentarily depressing the push button. If you forget to turn off the 811-BTS, an internal timer will turn it off after about 5 or 6 minutes. When the 811-BTS is turned on, the light in the push button will blink if the battery needs recharging. The instrument should be recharged as soon as possible after the light first begins to blink. However, the instrument will operate for about another hour after the light indicates charging is needed. We recommend you keep this unit on charge when it is not in use. You will get longer, more reliable service from the battery.
BOTH INSTRUMENTS VOLUME: This knob controls the loudness of the instrument. PROBE: The probe is connected to these two jacks. It does not matter which side of the probe is connected to which jack. The actual operating frequency of the Doppler is indicated by the probe jacks on the instrument and the frequency of the probe you use must match this number. The frequency of the probe is engraved on the probe body. When ordering new or different probe types, be sure to order by the frequency indicated on the instrument. Parks Medical Electronics, Inc. Models 811-B and 811-BTS
7
Front Panel Description Models 811-B and 811-BTS
CHARGER: This jack is used to recharge the internal battery. The charger supplied (Parks charger part no. 984-0006-02) is connected to the charger jack. When the charger is connected and plugged into an appropriate AC outlet, the battery is charging if the light by the charger jack is illuminated. The instrument will not turn ON when the battery is being charged. A safety lockout relay prevents operating the instrument directly from the charger and this circuit must not be changed or by-passed by the user. For safety reasons the charger must be disconnected when the instrument is used on a patient. The battery cannot be overcharged. Leaving the battery discharged for days will shorten the life of the battery. You can expect a life of 2 to 3 years for the battery with normal service and care. If you believe the battery is getting weak, keep the volume low or use headphones to get the maximum Doppler operating time before recharging or replacing it. EARPHONES: This jack is used to connect optional stereo headphones to the instrument. The headphones are a low impedance type. The speaker is disconnected when the headphones are plugged in. You always hear more using headphones, especially when you are checking weak flow or veins. The speaker in the instrument will not reproduce low-frequency sounds as well as the headphones. Low pitched sounds are associated with low-velocity flow. PROBE TYPES AVAILABLE: This instrument is designed only for vascular work, not obstetrical service. It can be used with the standard 3/8” diameter pencil probe, the “skinny” pencil probe (1/4” diameter), the infant flat and the adult flat probes.
The Coupling Gel YOU MUST USE GEL IN FRONT OF THE PROBE. We recommend you use a coupling gel made especially for ultrasound. Don’t use a gel that is too runny. You can use sterile jellies internally. Ultrasound coupling gels are available from us, or will usually be available from one of your surgical supply dealers. These gels are available in bulk, sterile packets and bottles. Gel in a semi-rigid tube with a small extended tip is easier to use than that which is in collapsible tubes. Refilling from bulk is much less expensive than buying more bottles or packets. Some tubes can be autoclaved. In an emergency use any sterile liquid or gel without excessive bubbles. Petroleum jelly or mineral oil can be used, but they often do not transmit the sound well. Sensitivity may be reduced and bubbles in the gel can make a popping noise. Placing the probe directly on wet tissue will also work. PLEASE DO NOT USE ECG PASTE OR CREAM. The probe crystals are covered by a material which is vulnerable to attack by heat, alcohol and ECG paste. THE RED PROTECTIVE COVER MUST BE REMOVED FROM THE PROBE BEFORE USE. DO NOT POINT THE ULTRASONIC BEAM INTO THE RETINA OF THE EYE. Based on experimental and epidemiological data, there is presently no identified risk associated with diagnostic ultrasound. However, a prudent and conservative approach is recommended in which diagnostic ultrasound should be used only for medical benefit and with minimal exposure. Extreme care should be taken when treating areas near the eye because of the danger of damage to the retina. Similarly, extreme care should be taken near the ears and reproductive organs.
103-0060-07
5/5/04
Parks Medical Electronics, Inc. Models 811-B and 811-BTS
8
Basic Operating Instructions USE OF THE PENCIL PROBE IN THE DIAGNOSIS OF ARTERIAL DISEASE IN THE LIMBS 1. THE PROBE. The probe consists of two crystals; one for transmitting the ultrasound waves and the other for receiving the reflected waves. If either crystal is damaged, the probe will not work properly or will not work at all. The crystals are covered by a material that is vulnerable to attack by heat, alcohol and ECG paste or cream. Therefore, DO NOT use ECG paste as the contact medium between the skin and the probe. Use AQUASONIC or any gel made for ultrasonic physical therapy equipment. In an emergency use any surgical jelly or lubricant, even petroleum jelly or mineral oil. Remove the gel after use with a soft tissue. If you should find the probe with dried gel on it, wash it off under running water. Do NOT scrape off the gel because you may damage the coating over the crystals. Do NOT autoclave the probe. Gas sterilization is the only acceptable method. 2. POSITION OF THE PROBE: Invariably, people not accustomed to our probe use it incorrectly. The probe we furnish is different from that of the other manufacturers and is used differently. If you hand someone the probe and say “Here, try it for yourself”, he will almost always put it over his radial artery and put the probe perpendicular to the artery-and perhaps with no coupling gel. Many people have tried to compare our Doppler with other makes by this method. Keep in mind that you are not buying a Doppler for use on the radial artery, but for use on vessels you cannot feel. The best testing ground is therefore in your particular area of interest. We believe our instruments will permit you to find the vessels easier, let you hear the venous sounds easier and follow the vessels better than any other device on the market, regardless of price. But it takes some practice in order to be able to do this. We believe the arm is a good and most convenient limb for you to learn on-to learn how to hold the probe depending on the depth of the artery and vein. The area about 6 inches each side of the elbow is a good place to start. First, put some gel on the tip of the probe. The gel squeeze-bottle must be shaken downward and then gently squeezed to get the gel to come out. Pile up about a quarter of an inch of gel on the probe, making certain there are no large air bubbles in the pile because ultrasound does not go readily through air. It needs a continuous conducting medium, and the gel is ideal. Turn the VOLUME control fully down (counter clockwise) and turn the instrument on. Gradually turn up the volume. You should hear a rumbling sound if you are holding the probe. This is caused by the vibration of the gel due to tremor in your arm. Now place the probe over an artery in the arm about half way between the elbow and the wrist. Tilt the back of the probe toward the hand at an angle of about 45 degrees, making certain there is gel in the pathway between the probe and the skin. Move the probe and the skin sideways to try to find the center of the artery and the hissing noise at heart rate, which is the Doppler sound for an artery. If the sounds you hear are more or less continuous, that is simply the background noise of the instrument and it means that you are not over the artery. The main energy of the beam is only about as wide as the crystals in the probe, so there isn’t much room for error in aiming the probe. For this reason you must always search the area of the artery and tilt the probe for best Doppler sounds. When you are looking for deep arteries, or for small or obstructed arteries, you will have to turn the VOLUME control near maximum. This also means that every time you move the head of the probe you are going to get some pretty big thumping noises in the earphones. Therefore you want to avoid moving the head of the probe with respect to the skin as much as possible. That is why you place the probe over the area where you think the artery is and then you search for the exact point by moving the skin with the probe and changing the angle of the probe with respect to the skin. You might wonder why these big transient noises can’t be filtered. We do limit their intensity, but we do not filter. The reason is that in the search for low-velocity blood flow, such as in occluded arteries and in the veins, the pitch of the Doppler sounds associated with the blood flow are very low. Any filtering to eliminate or minimize the sounds accompanying movement of the probe would also reduce the response to low-velocity blood flow sounds, and of course this is undesirable.
Parks Medical Electronics, Inc. Models 811-B and 811-BTS
9
Basic Operating Instructions
3. DIAGNOSIS OF ARTERIAL DISEASE: The Doppler method of diagnosing arterial disease of the limbs is only one of several good methods. It is probably the most convenient and least expensive of the better methods. It is only qualitative but can be made semi-quantitative by permitting you to make systolic blood pressure measurements along the leg with the aid of a proper cuff and manometer. The great sensitivity of the transcutaneous Doppler can cause a doctor or technician to conclude improperly that an arterial pathway is open when it isn’t. Collateral flow around an obstruction can be well-developed, especially in the thigh, and cause pulsatile blood to flow in the distal arteries. Or a major artery may be narrowed, causing pulsatile flow distally. These mistakes in diagnosis can be avoided almost entirely by simple means and a little bit of experience. An experienced user of the Doppler can recognize the characteristic sounds of open and obstructed arteries. Remember that Doppler sounds vary in pitch (frequency) with the velocity of blood flow. When you hear the Doppler sound on a normal artery and compare it with a normal arterial pulse-pressure wave, you will recognize the sound of the dicrotic notch, the very fast rise time of the wave and perhaps a third sound just before the onset of a new pulse wave. While the origin of these second and third waves in the descending branch of a pulse wave may be in dispute, their absence in vessels distal to an obstruction is not disputed. So a diagnostic rule is that whenever you hear the second and perhaps third sounds of a pulse wave of a major artery, you can be sure the artery is open proximal to the probe. Plethysmographic studies also show a delayed crest to the wave, associated with a slower rise time to the wave when there is an obstruction proximally. Though the Doppler is permitting you to hear velocity changes rather than true volume changes, the correlation is good enough to be quite valuable diagnostically. Now the opposite is not necessarily true-that when you can’t hear second and perhaps third sounds the artery is obstructed proximally to the probe. In the digits and smaller vessels the pulse wave is smoothed out more, especially when there is some vasoconstriction. Now of course there are cases that are in doubt. If you cannot clearly hear the second and third sounds (the third sound is frequently missing), compare with the same artery on the other limb. If you find a radical difference in the sound of the Doppler, both in pitch and in amplitude, you are justified in being quite suspicious of the patency of the artery of the first limb you studied provided you are now fairly skilled at optimizing the sounds. Another thing you listen for is the relative clarity of the arterial wave. How well it stands out from the background noise of the instrument and perhaps the venous flow adjacent to the artery. Move the probe a little to each side of the artery to make this estimation. In a normal person you will find that you can make the arterial pulse wave almost completely separate from the venous sounds by positioning of the probe. The way you really come to a final conclusion that the artery is obstructed proximal to the probe is by measuring the systolic pressure at the ankle with an ordinary arm cuff. If you want to measure pressure at other places on the leg you will need a special cuff, the bladder of which encircles the limb. We sell such cuffs. The method is as follows: Wrap the cuff around the ankle or slightly above it so you can get the probe on the posterior tibial and hear the arterial sounds adequately. Inflate the cuff to a pressure well above the patient’s arm pressure or at least 30 points above the pressure at which the Doppler sounds disappear. Gradually reduce cuff pressure until you hear blood flow, though the sound will not be normal. At that point read the pressure to obtain systolic pressure at the ankle. If you have doubts, center the probe on the artery and inflate the cuff again. You can observe at what cuff pressure the blood flow stops and again where it starts. Where it starts is normally used.
Parks Medical Electronics, Inc. Models 811-B and 811-BTS
10
Basic Operating Instructions
What you are doing is very similar to taking pressure on the arm using a stethoscope. There you are using sounds of turbulence or wall motion. Here we are sensing the flow of blood under the cuff with a much more sensitive device. You can get a clear indication of systolic pressures as low as 30 mm of Hg. The only problem is keeping the probe right on the center of the artery while you are inflating and deflating the cuff. An aneroid manometer mounted on the inflation bulb of the cuff is preferable. Tycos makes such a device and perhaps others do too. The possibility of misdiagnosing is greatly reduced by this method provided you make two or more measurements and you are skilled at holding the probe in the right place and at the right angle. A low pressure reading is quite reliable. On diabetics you may get readings of 300 mm Hg or more, even though they have ulcers on their toes. These people with end-artery disease studied plethysmographically with the mercury-in-silastic strain gage, which we also make, will have quite large and normal looking pulsations in the toes. Their arterial walls are sclerosed so badly sometimes that they will not compress with cuff pressure. The normal pressure in the ankles should be about the same as the systolic pressure in the arm, or a little higher. If the ankle pressure is 30 mm or more lower than the arm pressure, an obstruction is almost certainly present. Normally one finds that people with arterial obstructions have pressures of 100 or less. If you have a proper cuff you can take pressures in the same manner (with the probe at the posterior tibial) just below the knee, just above it and at the top of the thigh. By measuring systolic pressure (the pressure measurement is always where the cuff is, not where the probe is) you will find radical differences between measuring sites if the obstruction is between them or you will find that pressures at corresponding points on the two legs are quite different. An exception is bilateral obstruction of the bifurcation of the abdominal aorta which may give you fairly symmetrical pressures on both legs. Unfortunately you cannot use the Doppler above the top of the thigh. The pressure measurements made on the thigh with a narrow cuff will be clinically useful, though not accurate. Once you have determined that there is an obstruction it is often desirable to determine just where it is. It is permissible to check at certain points provided you are quite familiar with normal sounds-second and perhaps third sounds. Start at the top of the thigh and listen for the normal arterial sounds. A little to one side you should hear venous flow varying with respiration. The adjacent venous flow assures you that you are indeed listening to a major artery. This is important because you can get beautiful sounds from a collateral that is aimed toward your probe and giving a tremendous Doppler effect. But a collateral follows a tortuous path and the venous sounds will not be found adjacent to it. If you have a little problem hearing the vein (and you shouldn’t over big veins) give the leg a slight squeeze distal to the probe to increase the velocity of the venous blood and make its pitch higher. As you follow the superficial femoral artery down toward the knee you will lose the sound, even on normals, in some parts of the path because of tendons or other anatomical obstructions between the probe and the artery. You should be able to pick it up again easily in the popliteal region. Your ear and concentration make a filter to extract wanted information from background noise that exceeds anything that can be done electronically. You can follow these small arteries distal to the knee and in some cases they can be followed all the way to the ankle and beyond. Keep in mind that some people don’t have a dorsalis pedis artery. If you are working on arteries in the foot, make sure they are dilated by immersing the foot in a bucket of warm water for a few minutes. Some people are vasoconstricted most of the time. They usually will dilate for a while after the immersion and in a few minutes be constricted again. Also they usually do not have arterial disease. To summarize, if you want to quickly determine the patency of the arterial system in the leg, pick up the posterior tibial and listen for 2nd and perhaps 3rd sounds. If you hear them, and you are sure you know the difference between normal and abnormal, go no further. If they do not sound normal or there is doubt, make a blood pressure measurement and compare it with systolic pressure on the other ankle and on the arm. To find the location of the obstruction you can listen with the Doppler, or using a special cuff you can make blood pressure readings farther up the leg. If the obstruction is in the iliacs you can note it by the Doppler sound distal to the obstruction or by a much lower than normal blood pressure at the top of the thigh as measured with the cuff and the Doppler. Parks Medical Electronics, Inc. Models 811-B and 811-BTS
11
Basic Operating Instructions
PRE-OPERATIVE AND POST-OPERATIVE use of the Doppler is very important. When the patient is on the table, measure systolic pressure at both ankles and record it. After blood is again permitted to flow measure both pressures again. The pressure on the operated leg should be UP compared to the pressure in the other leg, the control. If it isn’t, then it is pretty safe to assume something is wrong. On rare occasions a limb will have such a high degree of reactive hyperemia that pressure will not be up and may even be lower, but the leg will be hot. A large percentage of patients are blocked to some degree before they get off the table. Blood-pressure measurements will give you an objective evaluation of the surgery. Some surgeons use the pencil probe directly on the artery (using sterile jelly for coupling) just distal to the repair. The characteristic of the flow sound is important. If the runoff is inadequate an experienced ear can detect it and often correct the cause on the table. You can also use Doppler and pressure measurements for follow up, comparing pressures at both ankles with systolic pressure at the arm, measured either with a Doppler or stethoscope.
105-0039-02
10/14/03
Parks Medical Electronics, Inc. Models 811-B and 811-BTS
12
Use Of The Flat Blood-Pressure Probes
Infant flat blood pressure probe
Adult flat blood pressure probe
We manufacture two different sizes of probes meant to be taped to the wrist for repeated blood pressure measurements. One is called the adult flat 15 degree or just adult flat. The other is the infant flat. The 15 degree nomenclature means that the crystals are set into the plastic so that the ultrasound beam goes into the vessel at about 15 degrees from perpendicular. The probes can be used on either adults or infants but the infant probe is definitely more convenient to use on infants because it is smaller. These probes must be obtained in a frequency (MHz) corresponding to that marked on your Parks Doppler. They are made in nominal 8 and nominal 9 MHz frequencies as standard probes. You should specify the actual frequency of your Doppler, such as 8.2 MHz, 9.4 MHz or whatever is marked by the probe jacks on your instrument. The beam width of these probes is about 10 mm, the longest length of the crystals. The probe is normally placed over the radial artery, where it is easiest to palpate, with the cord lying across the hand. This makes the crystals point upstream a little bit (15 degrees from perpendicular). There must be a gel contact between the skin and the material covering the rectangular crystals visible in the probe. In time, this gel can melt away, especially if the skin is sweaty, so if you lose signal, suspect that the gel is not bridging the gap between the skin and the crystals. Holding the probe in position can be a problem. Normally tape is used. If you first draw the skin up around the sides of the probe before putting the tape on it may stay in position better. Normally you anchor the cord in at least one place distal to the probe so it will not tug on the probe. A Velcro strap has been used by some. GENERAL INFORMATION ON MAKING THE MEASUREMENT OF SYSTOLIC PRESSURE: A Doppler is normally used to make accurate systolic pressure measurements. Diastolic pressure can be estimated by other sound changes in some cases, but it is not accurate. The accuracy of the systolic measurement depends on having the proper width cuff for the limb. The Doppler is merely serving as a sensing device to let you know that blood is spurting through the constriction in the artery imposed by the cuff. This corresponds to the first sounds you get through a stethoscope when you deflate the cuff. Since blood flow causes a hissing sound in a Doppler, you will clearly hear the hissing spurt of blood as cuff pressure is slightly lower than arterial pressure. You read the manometer on the cuff when you first hear blood flow sounds from the Doppler. The Doppler probe can be anywhere distal to the cuff. The measurement made is for the pressure at the site of the cuff, not where the Doppler probe is. TO MEASURE SYSTOLIC PRESSURE: First you put the cuff on the arm in the normal position above the elbow. You position the probe over the radial artery before you inflate the cuff and find where the flow is loudest. Then you anchor the probe with tape by manipulating the skin up the side of the probe before you tape. Next you inflate the cuff quickly to above estimated systolic pressure, letting the pressure down slowly. When you hear the spurt of sound from the Doppler, read the manometer and then deflate the cuff. Your manometer reading is the systolic pressure measurement. Parks Medical Electronics, Inc. Models 811-B and 811-BTS
13
Use Of The Flat Blood-Pressure Probes
The reason for using the Doppler and not a stethoscope is that the Doppler will allow you to make accurate systolic pressure measurements on patients with very low blood pressure, on legs, on fingers, rat tails, animal legs, dog and cat tails, etc. Again, accuracy depends on having the right width cuff. Systolic pressure measurements as low as 10 mm of mercury have been made on infants in surgery. DISCUSSION: The measurement is usually quite consistent with some experience. Variations in intrathoracic pressure can cause flow sounds to come and go when you lock the manometer to a specific pressure, such as 145. When you are in doubt about a pressure, lock the manometer at some reading and see if there is a spurt of flow with each cardiac cycle. Increase pressure a bit and see if the spurt stops or only occasionally comes through. Normally when the spurt of flow is there for 2 cardiac cycles as you lower pressure, that is the measurement you want. Oscillation of the needle on the manometer is not a valid measurement. Diabetics, whose arteries may be calcified, may give you high systolic pressure readings, especially on the legs. This would happen with a stethoscope too. You cannot make an accurate systolic pressure reading using a cuff when arteries at the wrist or ankle are heavily calcified, regardless of whether you use a stethoscope or a Doppler. CARDIOPULMONARY BYPASS MEASUREMENTS: When a patient is on cardiopulmonary bypass or there is some type of shunt between the artery and vein, there is no pulse. What you must do is inflate the cuff to above systolic pressure, let pressure fall rather quickly and note the pressure in the cuff when you first hear blood flow sounds from the Doppler. DIGITAL AND TAIL MEASUREMENTS: Animal and tail vessels can constrict so completely that the blood just oozes, it does not pulsate. Therefore you cannot detect it with the Doppler because the velocity is too low. You must release vasomotor tone by warming or causing tissue anoxia (inflating the cuff to above systolic pressure and leaving it at that pressure for 5 minutes or so). DIASTOLIC PRESSURE MEASUREMENTS: The Doppler method is not very suitable for diastolic measurements. The reason is that the diastolic measurement is a cessation of the vibration of the arterial wall. In normals, this is easily heard with a stethoscope. As pressure falls or the limb is small, the stethoscope does not work either. You can estimate diastolic pressure in two ways. One is to insert the probe under the lower edge of the cuff and listen for the disappearance of the thumping sound as you pass diastolic pressure. The problem with this is that positioning of the probe so it will stay in place is often difficult. Also the distance to the brachial artery on obese or muscular people may be so great you cannot get a good Doppler sound. What some people do is use the probe at the radial artery as above noted, but listen for the return of the dicrotic notch, where flow signal is first heard during the entire cardiac cycle rather than an interrupted sound. These measurements are estimates and we do not claim accurate diastolic readings can be made. STERILIZATION: Cold sterilizing solutions can be used for the prescribed time limits set by the manufacturer, but they do NOT sterilize the probe. If you choose to cold sterilize, wash everything in running water and hang or wipe to dry. Also, it is best not to insert the connectors into the solution. Alcohol will soften the material covering the crystals and eventually destroy the probe, so do not soak the probe in alcohol and do not autoclave because heat destroys the cable and the crystals. Gas sterilization (ethylene oxide) is the only proven method of sterilization. Temperatures above 140 degrees Fahrenheit (60 degrees Celsius) can ruin the probes. PROBE CARE: Repeatedly disconnecting the probe from the unit will eventually wear out the connectors in the panel of the instrument, causing “static”. Repeated flexing of the cable near the plastic probe body will eventually destroy the cable shielding and also cause “static”. It is always best to have a spare probe because should you have a problem with the instrument and not have a spare probe, you will not know whether the probe or the Doppler is at fault. If you have a spare, you will know immediately whether simply replacing the probe will cure the problem. Having a spare probe could eliminate having to send the entire instrument to the factory for service. Parks Medical Electronics, Inc. Models 811-B and 811-BTS
14
Technique Of Evaluating Calf Venous Disease
The assessment of calf venous disease by Doppler ultrasound may be achieved with an accuracy of up to 85% compared to venography when one is experienced with the technique. The status of the calf veins can be assessed by listening with the Doppler at the posterior tibial vein at the ankle, the popliteal vein, the superficial femoral vein, and the common femoral vein. The status of the calf veins is determined by a combination of augmentation maneuvers when listening at these various points. Normal Respiration Flow Sounds: The Doppler is initially placed over the posterior tibial vein at the ankle behind the medial malleolus. Generous amounts of acoustic gel must be used, and one must be careful to avoid undue pressure with the probe which might result in obstruction of venous flow. Initially the posterior tibial artery signal is elicited. The probe is then moved slightly to either side of the arterial signal until the windstorm like venous signal is heard. Normally this signal should wax and wane with respiration. In the presence of calf vein thrombosis, the signal may be more continuous or there may be no audible signal present. If the feet are vasoconstricted, a venous flow signal may not be heard until the venous velocity is increased by gentle compression of the foot. Checking Competency of the Valves: Once the optimal venous signal is elicited, the calf is then compressed with the hand which is not holding the probe. The fingers should be spread so that much of the calf muscle is compressed. During this procedure, no venous flow should be heard. If venous flow signals are elicited, this is a sign of deep venous valvular incompetence, usually secondary to old deep vein thrombosis. Augmenting Venous Velocity by Compression: Next the calf is released and one should normally hear an augmentation of venous flow as blood enters the previously decompressed calf veins. The magnitude and duration of the augmented signal can be influenced by several factors including the temperature of the foot, the general vasomotor tone of the patient and the presence or absence of venous thrombosis in the calf. It is important to compare the augmentation signals in each foot. In vasoconstricted individuals with cold feet, the posterior tibial venous augmentation may be very minimal but it should be symmetrical. If there is good augmentation in one leg and poor augmentation in the other, the latter leg is usually the site of venous thrombosis. Next, the common femoral and then the superficial femoral veins are examined and the signals assessed for augmentation upon calf compression. Calf-vein thrombosis will result in a decreased augmentation of the venous signals at these sites. Similarly the popliteal vein should be examined. In general, the most sensitive indicator of calf-vein thrombosis is a relative decrease in augmentation upon release of calf compression with the probe positioned over the posterior tibial vein at the ankle. There are certain conditions which will imitate calf-vein thrombosis. Such problems as subfascial hematoma, a ruptured Baker’s cyst, extensive edema, or other conditions which cause increased pressure on the calf veins may result in a decreased augmentation of flow during the aforementioned maneuvers. Such conditions can be best diagnosed by a venogram if the diagnosis is in question.
109-0003-01
12/10/02
Parks Medical Electronics, Inc. Models 811-B and 811-BTS
15
Using The Doppler On Digits
1/4” “Skinny” Pencil Probe
Standard 3/8” Pencil Probe
The Doppler normally comes equipped with a 3/8” nominal 8, 9 or 10 MHz pencil probe. There is little if any difference in the performance of probes operating at these frequencies. At lower frequencies, such as 4 or 5 MHz, the efficiency of the ultrasound signal is poorer and performance on surface vessels will not be as good as it is with a higher frequency probe. We also make a 1/4” skinny pencil probe which some people like for digits and supraorbital arteries. The benefit is better separation of artery and vein. Mostly the two lie close together, and you will find supraorbitals much easier to do with the skinny pencil. You will also find that you get a better signal-to-noise ratio in many cases. Line up the long way of the crystals and the pencil probe body with the length of the artery for best separation of arteries and veins at the ankle and best efficiency on the digital arteries. Whenever you try to pick up arterial flow from the digits you must consider digit temperature. It is often difficult to get a digital pulse when feet are cold or cool. The digits can be so vasoconstricted that blood only oozes through, which is sufficient to nourish but does not give a good recording or sound on any device. This occurs in perfectly healthy digits under normal conditions. It also occurs after surgery when severe vasospasm may occur. In order to get a good sound or blood pressure measurement under these conditions you must cause vasodilatation to take place. One method is to warm the extremity by immersing it in warm water, not hot water. Within a few minutes you will be able to evaluate the condition of the flow when the limb is at heart level or slightly above. Another method used to dilate peripheral vessels is to occlude all flow at the ankle or forearm with an ordinary arm cuff inflated to well above systolic pressure. This is not normally painful, especially when vascular disease is present in the arterial system. If too much discomfort is apparent, a different procedure could be tried. Five minutes is usually enough time. On release of cuff pressure a reactive hyperemia will take place and last for a short time at least. There should be enough time to make an evaluation of arterial patency. Diabetics may have incompressible arteries so this technique may not work with them. When there are two sounds to the arterial pulse wave, the first caused by the filling of the vessel with systole and the second being either forward or reverse flow in the diastolic phase, vessels are usually patent.
However, blockage of major proximal arteries may be present with good collateral flow around them. When there is only one sound with each cardiac cycle and the sound is not brisk, a proximal stenosis or occlusion may be present. PROPER PROBE PLACEMENT AND PROPER USE OF GEL ARE VERY IMPORTANT! The pencil probe body should be in line with the artery, not crosswise to it, and should be at about a 45 degree angle. You must be very careful about probe pressure, because a slight amount of pressure against the skin will occlude the artery. You must use a dab of gel in front of the probe. You may find it impossible to make blood pressure measurements on the digits with a Doppler, especially the toes. It is better to use our photoplethysmograph for that purpose. Doppler sounds from digital arteries will be very helpful once you become familiar with normal and pathological sounds. Making digital pressure measurements on the toes is not a very popular procedure. Refer to your medical literature for diagnostic procedures. This information is primarily meant to be a simplified guide to the use of the instruments and the probe. 109-0018-22
12/8/03
Parks Medical Electronics, Inc. Models 811-B and 811-BTS
16
Strange Noises From The Doppler
On occasion there are noises you might not expect from the Doppler when in fact the Doppler is working fine. The following are some common concerns and their causes.
Concern:
Cause:
Remedy:
Popping scratchy noises sounds when the probe is first placed on the skin.
Air bubbles in the gel are moving and / or popping. Hair movement can also cause these noises.
Use a new dab of gel that looks clear, push the probe down enough so hair is immobilized, and wait a few seconds for everything to settle. If the noise is not there when the probe is clean (no gel) and suspended in the air, the Doppler and / or probe are probably working fine.
Static when the dry probe is moved through the air.
Loose connectors where the probe connects to the instrument, broken shield wire in the cable either at the connector or as it comes out of the probe.
There is normally some static generated when the cable is flexed, but it isn’t severe. Replace probe or get connectors fixed. If the problem persists contact the factory.
High pitched tone and flow indicators (if so equipped) go to the extreme.
Radio interference from a mobile service, police station nearby, even another Doppler working close by. Usually occurs near large open windows, rarely in the center of the building.
Move the Doppler to another location away from windows and toward the center of the building. If the problem persists contact the factory.
Buzzing noise that almost obliterates the Doppler signal.
Electrocautery or other sparking device, bad fluorescent light fixture or neon signs nearby.
Move the Doppler to another location away from the interference. If the problem persists contact the factory.
Howling noise when probe is held or laid on a table with gel on it.
Probe is acting as a microphone and you are getting acoustic feedback.
Wipe gel from probe, If the noise does not occur without gel on the probe, it is probably working fine.
ADDITIONAL TESTS: 1. Try using headphones if you have a howling noise. If there is no howl using headphones, but there is with a speaker, it is acoustic feedback. 2. Try a different probe. Even if it is the wrong frequency it will let you know if the problem is noisy connectors in the instrument or frayed shielding near the probe body. SUMMARY: The problem may simply be a probe or it may be peculiar to the environment in which it is used. If you have tried the tests and remedies mentioned and you still suspect a problem contact the factory toll-free at 1-800-547-6427. 107-0027-04
4/97
Parks Medical Electronics, Inc. Models 811-B and 811-BTS
17
Care Of The Probe And Sterilization
The Doppler probes are easily ruined through misunderstanding and neglect. Over 90% of the failures of the Doppler are due to failure of the probe in some way. It will pay you to read what follows and transmit this information to any person using the Doppler. ABOUT THE PROBE: The active part of the probe consists of two crystals. One transmits the ultrasonic waves and the other receives them. Each crystal can serve either function so it makes no difference how you plug in the probe to the panel connectors. The crystals are held in place by a material that protects the crystals and the tiny wires soldered to them. This material is vulnerable to attack by heat, alcohol and ECG paste. We recommend an ultrasonic gel but in an emergency, use any surgical jelly. DO NOT use ECG paste or cream as a contact medium between the skin and probe. After use, the probe should be gently wiped clean of the Aquasonic or other acoustical coupling gel with a soft tissue. If the gel has dried on the probe, put it under running tap water (not hot) to soften the gel and permit you to wipe it off. Should someone use a sharp instrument to scrape off dried gel, they may also succeed in scraping off the material covering the tiny wires and crystals as well. We speak from long experience. Such probes cannot be repaired, and in fact any probe with a broken or cracked crystal cannot be repaired. You must order a replacement, specifying the frequency marked on the connecter (something like 9.2, 8.1, etc.). BE SURE THE PROBE FREQUENCY MATCHES THE TUNING OF THE INSTRUMENT. The frequency of the probe is marked on the connector end of the cable or engraved on the metal of a pencil probe. The tuning of the instrument is marked with a stick-on label near the probe connectors. DISCONNECTING THE PROBES from the instrument should be minimized. Don’t do it unless you need to, for two reasons. First the connectors wear and make erratic contact after many disconnects. Second, people have a tendency to pull on the cable instead of the connectors themselves and they break the soldered connection inside the cable connector. THE COUPLING GEL which we furnish is called Aquasonic, made by Parker Laboratories. This gel is available from us or a similar ultrasonic gel (not runny) will usually be available from one of your surgical supply dealers. The .25 liter bottles may be autoclaved. Other makes of gel may work as well, though the dispenser may not be as convenient. Coupling gel in sterile packets is also available from us. You can also use sterile jellies internally such as K-Y or ABCO. Any sterile liquid or gel without excessive bubbles may be used. Placing the pencil probe directly on wet tissue will also work. STERILIZATION: Cold sterilizing solutions can be used for the prescribed time limits set by the manufacturer, but they do NOT sterilize the probe. Sterilizing should be done by gas (ethylene oxide) at the lowest temperature consistent with good sterilization. Limit the temperature to 140 degrees Fahrenheit (60 degrees Celsius). Excessive heat will ruin both the crystals in the probe and the cable. Possible consequences are softening of the material covering the crystals with subsequent peeling and / or excessive noise generated in the probe from deposition of chemicals inside. A sterile water rinse after chemical sterilization is recommended. Sterilization of our standard pencil, skinny pencil, adult and infant flat probes has been tested by STERAD with their equipment and has been found satisfactory from reports we have received from them. Sterilization by any method is going to shorten the life of the probe, but the cost per use is quite low. Expect at least ten sterilization cycles of the probe. A PROBE EXTENSION CABLE may be purchased which allows you to keep the Doppler out of the sterile field when the probe is to be used intraoperatively. This cable is about four feet long and costs very little.
107-0000-11
10/17/03
Parks Medical Electronics, Inc. Models 811-B and 811-BTS
18
General Maintenance Of The Doppler MODELS 811-B AND 811-BTS
Notes For The Service Technician In addition to true service problems, you will frequently encounter “operator trouble”. Things to watch out for are: 1. The Doppler is tuned to a frequency that is different from that marked on the probe. This occurs in hospitals which have Dopplers and probes of more than one frequency. The probes and instruments get mixed up. We try to circumvent this by sending a particular hospital Dopplers and probes of the same frequency. The probe frequency is marked on its connector and the Doppler frequency is marked with a stick-on label next to the probe connectors or on a label elsewhere on the instrument. A variation of .1 MHz is not significant at around 5 or 10 MHz, but it is around 2 MHz. 2. The battery is either the wrong type or was put in backward or was shorted while being installed. The result is diminished battery life. 3. An attempt is made to feed the signal from the earphone plug on the Doppler to another device for either amplification or processing and it does not work. The most likely reason for this is that a single ended plug has been used which shorts out the stereo-type jack in the Doppler. You must use a tip-ring-sleeve-type plug (stereo) to take off the audio signal. True service problems can be broken down into the following general categories which are listed in the approximate order of their occurrence. 1. Failure of the probe. This accounts for about 90% of all the service problems. The user should keep a spare probe of the proper frequency on hand if they depend on the Doppler. 2. Probe connectors or panel jacks are making poor contact and there is “static”. The center pin wiping on the panel jack is usually at fault. A sharp tool can be used to bend the wiping sleeve inward and stop the noise. 3. Failure of the low battery warning light, battery or case because the instrument was dropped. 4. Leaking battery has corroded battery terminals so that good contact is not made or corrosive fluid has penetrated end insulators causing electrical leakage to ground. 5. Component failure, un-soldered joint or poorly soldered joint, wire to battery or connector broken (perhaps only internally). Look for broken resistors around the edge of the circuit board. They may be broken inadvertently during the process of changing the battery. In general we suggest you return the unit to us for service that might be complicated or that may require transistors. The reason is that transistors are often selected for low noise or their dc operating characteristic. Customers in the U.S. can call the factory toll-free at 1-800-547-6427. In Oregon, our local business phone is 503-649-7007.
Manufactured in the U.S.A. by:
PARKS MEDICAL ELECTRONICS, INC. 19460 S.W. Shaw, Aloha, OR 97007 1-800-547-6427 or 503-649-7007 Fax - 503-591-9753 107-0001-54
1/8/04
CE Units Available for European Market Visit our Web Site at - www.parksmed.com
Parks Medical Electronics, Inc. Models 811-B and 811-BTS
19
Service Information This information is meant to help the technician with common service problems.
COMMON PROBLEMS: PROBE AND PROBE CONNECTORS: Component failure is rare, consequently the probe connectors will most often be the problem. Example; the connector on the panel does not wipe the center pin. With no gel on the probe, you can jiggle the connectors and see if you get static. Use an awl or large needle to bend the edge of the wiping sleeve inward (panel jack). When the probe connector is lightly inserted, it should stop before the outer flange engages the probe jack on the panel. This means it is encountering resistance at the tip of the center pin, which is what you want to happen for a wiping action. Some probes fail because of the solder joint on the crystal. Sometimes it is visible, sometimes not. You can check for this by using a scope to look at the exciting voltage on the transmitting connector. It should be at least 4 or 5 volts peak-to-peak with a load. If you plug in the probe and the voltage drops, you know the probe is loading it. If it does not drop but a small amount (capacitive loading of the cable), then the crystal may be disconnected internally. Compare the two crystals for loading. The wrong frequency probe is being used, check to see that the frequency on the stick-on label by the probe jacks matches the frequency marked on the probe. The probe may have been damaged by soaking it in alcohol or a conductive sterilizing solution, or the probe has been damaged by autoclaving it. Dried gel on the probe may have been scraped off with a knife, damaging the crystals or the tiny wires leading to them. Also failure to take the red protective cover off the probe. STATIC PROBLEMS: Users often complain of “static”. ALWAYS CHECK FOR STATIC WITH NO GEL ON THE PROBE. Wiggle the wires near the panel and near the probe. Common causes of “static” are hair on the body, air bubbles in the gel popping, and sometimes radio interference (includes diathermy, electrocautery, NMR). All tests for static or interference should be done with no gel on the probe and with pencil probes being held in the hand or on an insulator because in high interference areas, touching the shield of the pencil probe carries R.F. signals into the box. If that problem exists, we make a special probe to eliminate that possibility. Sometimes a doctor complains about intraoperative use. If you can not make the instrument act up outside the O.R., You either have interference or operator problems. The technician without Doppler experience cannot know how to test for sensitivity of the total system. Those of us who have tested thousands of Dopplers may have differing opinions at times. That is why it is best to return the instrument to the factory if there is a sensitivity problem replacing a probe does not cure. But don’t do so without first calling us. We can handle many service problems over the phone and we are glad to do so.
107-0019-08
10/28/03
Parks Medical Electronics, Inc. Models 811-B and 811-BTS
20