Smith & Nephew
RENASYS TOUCH Clinician User Manual Rev 11
Clinician User Manual
525 Pages
Preview
Page 1
*smith&nephew RENASYS™ TOUCH Negative Pressure Wound Therapy
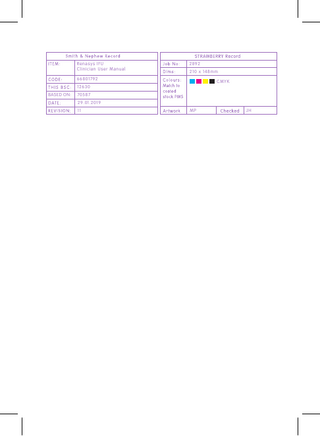
Clinician User Manual REF 66801791
BLANK
*smith&nephew RENASYS™ TOUCH
Clinician User Manual REF 66801791
Negative Pressure Wound Therapy
Table of contents Pause Therapy Lock/Unlock feature
16 16
End Therapy
16
11
Settings Alarm volume Compression rate Change Mode Language Set Date and Time Time Zone Flow Meter Send Data Restore Presets 3G and GPS Device Information
17 17 17 17 18 18 18 18 18 19 19 20
Canister selection
11
Pump Activity Log
20
Installing canister
12
Removing/changing canister
12
Turning on device
13
Navigating the touchscreen interface
13
Help Alarms/Troubleshooting Quick Reference Guide Video Guides Customer Assistance About
20 20 21 21 21 21
Setting therapy Set Y-Connect Set Therapy Mode
14 14 14
Starting therapy
15
Alarms/troubleshooting Over Vacuum Alarm High Vacuum Alarm Low Vacuum Alarm Leak Blockage Canister Full Low Battery Critical Battery Battery Failed Device Failed Inactive Annual Maintenance
22 23 23 24 25 26 27 27 28 28 28 29 29
Introduction
5
Important information Monitoring NPWT
5
Indications for use
5
Contraindications
5
Warnings
6
Precautions
6
Physician orders
8
Device description
9
Device orientation during use
10
Dressing changes
Table of contents (continued) Accessories IV pole/bed clamp Carry bag Carry straps
30 30 31 32
Maintenance Cleaning Disinfecting
33 33 33
Annual Maintenance
33
Battery operation and charging
33
Returning the device
34
Storage and battery maintenance
34
Electromagnetic compatibility
35
Radiofrequency radiation exposure information
36
Antenna Statement
36
Specifications
37
Intended location of operation
39
Replacement parts and accessories
40
Caution statements
41
Essential performance
41
LIMITED WARRANTY
42
Icon and symbol glossary
43
Global customer assistance
519
EN accumulation within the wound, which could lead to maceration, infection, or unrecognized bleeding.
Introduction This user manual contains important information regarding the safe and effective operation of the RENASYS™ TOUCH Negative Pressure Wound Therapy (NPWT) device (REF 66801791). This device is intended for use by or on the direction of a trained and licensed physician. This manual is intended to aid in the training of personnel and to provide a reference for experienced users. Also included are instructions for operating device, preventive maintenance, cleaning and return.
Monitor the wound for infection and ensure that all wound filler is removed at each dressing change to reduce the risk of infection. Skin grafts should be closely monitored to ensure NPWT is being delivered. Review Contraindications, Warnings & Precautions before use.
Indications for use
The RENASYS TOUCH is intended for use in acute care settings and other professional healthcare environments where product use is conducted by or under the supervision of a qualified healthcare professional.
RENASYS TOUCH is indicated for patients who would benefit from a suction device (Negative Pressure Wound Therapy), as it may promote wound healing via removal of fluids, including irrigation fluids and body fluids, wound exudates and infectious materials.
RENASYS TOUCH is also intended for use in residential settings and nursing homes where product use is conducted by or under the supervision of a qualified healthcare professional.
Appropriate wound types include:
To ensure that the device is safe for use in residential settings, this device is compliant with the IEC medical equipment and medical electrical safety standard 60601- 1-11 for use of medical devices in the home healthcare environment. This standard includes the use of a double insulated Class II power supply and Class II power cord.
•
Chronic
•
Acute
•
Traumatic
•
Sub-Acute and dehisced wounds
•
Ulcers (such as pressure or diabetic)
•
Partial-thickness burns
•
Flaps and grafts
Contraindications
Important information: Monitoring NPWT
Use of RENASYS TOUCH is contraindicated in the presence of:
Carefully monitor the patient, device, and dressing frequently to determine if there are any signs of bleeding, exudate accumulation (pooling), infection, maceration, or loss of Negative Pressure Wound Therapy (NPWT). The frequency should be determined by the clinician based on individual characteristics of the patient and wound. NPWT devices are not designed to detect or issue an alarm condition based on the presence of bleeding or pooling. These conditions may only be detected by frequent monitoring. Special attention to the risks of bleeding or loss of NPWT should be considered when prescribing for use in the Home Environment. NPWT may be impacted by various conditions related to system configuration, set-up and individual characteristics of the patient and wound (e.g. exudate characteristics, patient anatomy). Alignment of the port to the opening in the drape, use of a bridging technique and choice of dressing configuration based on wound characteristics may impact NPWT vacuum delivery over the course of therapy. Exudate volume, viscosity and consistency may influence fluid removal or occlusion formation. A full canister, incorrect device orientation and device/tubing height relative to the wound can contribute to loss of NPWT and exudate 5
•
Untreated osteomyelitis
•
Exposed arteries, veins, organs or nerves
•
Necrotic tissue with eschar present
•
Malignancy in wound (with exception of palliative care to enhance quality of life)
•
Non-enteric and unexplored fistulas
•
Exposed anastomotic sites
EN
Warnings
Precautions
1. Carefully monitor patients for signs of bleeding,
1. More frequent device and wound dressing
which may lead to interruption in therapy and hemodynamic instability. If such symptoms are observed, immediately discontinue therapy, take appropriate measures to control bleeding, and contact treating clinician.
monitoring should be undertaken for patients who are or may be:
• Suffering from infected blood vessels • Receiving anticoagulant therapy or platelet aggregation inhibitors, in addition to patients with intrinsic coagulation problems such as low platelet counts
2. Patients suffering from difficulty with hemostasis
or who are receiving anticoagulant therapy have an increased risk of bleeding. During therapy, avoid using hemostatic products that, if disrupted, may increase the risk of bleeding.
• Actively bleeding or have friable blood vessels or organs • Suffering from abnormal wound hemostasis
3. Do not use directly on exposed blood vessels or
organs. Sharp edges such as bone fragments must be covered or removed prior to initiating therapy, due to risk of puncturing organs or blood vessels drawn closer under the action of negative pressure.
• Malnourished • Noncompliant or combative • Suffering from wounds in close proximity to blood vessels or friable fascia.
Patient size and weight should be considered when prescribing the device.
When monitoring patients for delivery of therapy, ensure wound dressing is free of air leaks, fully compressed and firm to the touch.
5. Foam or gauze must not be tightly packed or
2. As a condition of use, device should only be used
4. NPWT has not been studied on pediatric patients.
by qualified and authorized personnel. User must have necessary knowledge of the specific medical application for which NPWT is being used.
forced into any wound area. Over-packing may interfere with distribution of NPWT evenly across the wound. This may decrease the ability of the wound to properly contract and permit exudate to remain in wound.
3. For patients with high risk of bleeding, use 300ml canister. Ensure the 300ml canister viewing is checked frequently for signs of bleeding.
6. In the event defibrillaton is required, disconnect
4. The dressing seal may be lost or pooling may
device from wound dressing only if its location will interfere with defibrillation.
occur, without alarm activation, when an occlusion forms on the wound side of the dressing. Viscous, purulent or serosanguineous drainage may contribute to occlusion of the dressing. Regular monitoring of device and dressing is required to ensure full delivery of therapy and exudate removal. Ensure the wound dressing is free of air leaks, fully compressed and firm to the touch whenever therapy is active.
7. Device is not MRI compatible. Do not bring device into MRI suite. Prior to entering MRI suite, disconnect device from dressing. Dressing can remain intact on patient.
8. Device is unsuitable for use in areas where there is danger of explosion (e.g., hyperbaric oxygen unit).
5. Underlying structures, such as bone, tendons,
9. When operating, transporting or disposing of
ligaments and nerves should be covered with natural tissue or a non-adherent dressing layer prior to applying the NPWT dressing to ensure protection and minimize the risk of damage from direct contact with the dressing.
device and accessories, there is risk of infectious liquids being aspirated or contamination of device assembly through incorrect use. Universal precautions should be observed whenever working with potentially contaminated components or equipment.
6. To minimize the risk of bradycardia, do not place NPWT in proximity to the vagus nerve.
10. Device and canister kits are provided non-sterile
7. In the event a patient with spinal cord injury
and should not be placed within a sterile field.
experiences autonomic dysreflexia, discontinue use of NPWT and immediately seek medical assistance.
11. When using a Y-connector, the system will only detect a blockage if both connections are blocked.
8. When treating enteric fistulas, do not place NPWT dressing in direct contact with exposed bowel.
6
EN Cover the wound bed, including fistula opening, with non-adherent gauze or with one layer of saline moistened gauze. Alternatively, consider isolating the fistula using an ostomy bag and dress the rest of the wound appropriately to avoid the wound being bathed in effluent from the enteric fistula. During the course of treatment patient’s fluid levels must be closely monitored.
RENASYS™ TOUCH device.
18. Ensure canister tubing and RENASYS Soft Port are installed completely and without any kinks to avoid leaks or blockages in vacuum circuit. Position device and tubing appropriately to avoid risk of a trip hazard. Device and system tubing should be positioned level with or below the wound to ensure optimization of therapy and prevent therapy interruption.
9. Avoid use of circumferential dressings except in
cases of oedema or heavily exuding extremities, where this technique may be necessary to maintain a seal. Consider using multiple drapes to minimize risk of decreased distal circulation. Regularly assess distal pulses, and discontinue therapy if changes in circulation are detected.
19. When bathing or showering patient must
disconnect from device, protecting both ends of tubing using tethered caps. Ensure aeration disc located near quick click connector is free of moisture before reactivation of therapy to ensure proper alarm functionality and prevent interruption in therapy.
10. Monitor patient for any signs of local or systemic
infection. Infected wounds may require more frequent dressing changes. As NPWT is not intended to directly treat infection, if there are any signs of systemic infection or advancing infection at wound area, contact treating clinician immediately.
20. If any liquids penetrate device, discontinue use and return to your Smith & Nephew authorized provider for service.
21. CT scans and x-ray have the potential to interfere with some electronic medical devices. Where possible, move device out of x-ray or scanner range.
11. If multiple pieces of foam or gauze are needed to
fill the wound profile, count and record how many pieces are present to ensure all pieces are removed at a dressing change to minimize the risk of retention and possible infection.
22. Do not use in the presence of a flammable
anesthetic mixture with air or with oxygen or nitrous oxide.
23. AC mains power can only be removed by
12. NPWT should remain on for duration of treatment.
disconnecting power cord or AC power supply. Take care in positioning the device to allow access to the power jack.
The length of time a patient may be disconnected from device is a clinical decision based on individual characteristics of patient and wound. Factors to consider include location of wound, volume of drainage, integrity of dressing seal, assessment of bacterial burden and patient’s risk of infection.
24. If power supply or power cord is damaged, wires
are frayed or exposed, do not use power. Contact your Smith & Nephew representative for a replacement.
13. Do not use a dressing kit with breached or
25. Canisters should be changed at least once a
damaged packaging.
week, whenever there is a change in patient or in the event that canister contents reach maximum volume indication (300ml or 800ml fill line). Do not wait for the Canister Full alarm to sound to change canister.
14. Use of NPWT presents a risk of tissue in-growth.
Tissue in-growth may be reduced by reducing therapy pressure, using a wound contact layer or increasing the frequency of dressing changes.
26. Canisters are single use. Do not reuse.
15. NPWT should not be painful. If patient reports
discomfort, consider reducing pressure setting and use of a wound contact layer. Pressure setting is a clinical decision based on individual characteristics of patient and wound. Factors to consider include location of wound, volume of drainage and integrity of dressing seal.
27. Do not apply SECURA™ No-sting barrier film wipes
16. Maintain regular monitoring of device and wound
28. As with all adhesive products, apply and remove
directly to open wounds. SECURA No-sting barrier film is flammable. Use in a well ventilated area. Avoid using around flames and sources of ignition. Keep out of reach of children. For external use only.
site during therapy to ensure therapeutic treatment and patient comfort.
dressing carefully from sensitive or fragile skin to avoid blistering and skin stripping, especially after frequent dressing changes. Use of skin sealant may assist with protection of periwound skin.
17. Device is only to be used with Smith & Nephew
authorized components. Use of any other products has not been proven safe and effective with 7
EN
29. If device must be disconnected, the ends of the
Physician orders
30. Due to its smaller diameter, the RENASYS™-G 10Fr
Prior to placement of RENASYS TOUCH, the medical professional treating the wound must assess how to best use the system for an individual wound. It is important to carefully assess wound and patient to ensure clinical indications for Negative Pressure Wound Therapy (NPWT) are met.
dressing tubing and canister tubing should be protected using tethered caps to avoid leakage of fluid and cross contamination.
Round Drain Gauze Kit and Accessory Kit are not recommended for use with RENASYS TOUCH, as reduced pressure in the wound bed may lead to pooling or maceration.
All orders should include:
31. The RENASYS TOUCH system compatibility with
• Wound location, size and type
diagnostic procedures is listed below. However care should be taken if the RENASYS TOUCH pump or RENASYS dressing is positioned in a location that will interfere with any of the procedures. Medical therapy/ diagnostic procedure
RENASYS Pump RENASYS Dressings
Defibrillation High Resolution X-Ray Computed Tomography (CT) Imaging
Compatible Compatible Compatible
Compatible Compatible Compatible
Fluoroscopy Ultrasound
Compatible Compatible
Compatible Compatible
Magnetic Resonance Imaging (MRI)
NOT Compatible NOT Compatible
Hyperbaric Oxygen (HBO)
NOT Compatible NOT Compatible
• Smith & Nephew Wound Dressing Kit • Pressure settings • Frequency of dressing changes • Adjunctive dressings
8
EN
Device description The RENASYS™ TOUCH device is designed to provide Negative Pressure Wound Therapy to a closed environment over a wound in order to evacuate exudate from the wound site to a disposable container, which may promote wound healing via removal of fluids, including irrigation of body fluids, wound exudate and infectious materials. The closed environment is created by applying a RENASYS sterile wound dressing to the wound site and connecting the sealed wound to the suction device. The RENASYS TOUCH device contains integrated global cellular technology that allows device location, billing and maintenance data to be sent to a secure Internet website providing clinical access to device information. The RENASYS TOUCH device has two main user interface areas: the full-color touchscreen and the three buttons below the touchscreen.
Front view of device Touchscreen
Status indicator
The three buttons below the touchscreen are used to power On and Off the device, Start and Pause Therapy, and Lock and Unlock the user interface. The status indicator at the top of device illuminates green when therapy is active or yellow to indicate an alarm state. The status indicator is not illuminated when therapy is not active. The RENASYS TOUCH device runs on AC mains power or can be used on internal battery power to allow the user greater mobility. Using the external AC power supply and power cord, the device can be plugged into an electrical (AC) outlet to charge the battery without causing interruption to active therapy. When the device is plugged in, the external power indicator next to the power jack illuminates green to indicate the device is connected to an external power supply. When the device is On, the battery indicator on the touchscreen will display a lightning bolt to indicate the battery is charging. RENASYS TOUCH is designed to be used with a RENASYS TOUCH power supply. Attachment knobs are located on the left and right sides of the device. These features are used to attach the carry strap and IV pole/bed clamp accessories. The rear of the device houses the speaker and identification label. The odor filter, USB port and air exhaust outlet are located behind the rear access door. The underside of the device houses the inlet port, replaceable o-ring and barcode label.
Power
Lock/Unlock
Start/Pause Therapy
Left view of device and power
Power cord inlet Power cord
External power indicator Power jack Power supply DC cord
Rear view of device Speaker
Attachment knob
Odor filter & USB access door Air exhaust outlet
66801791
Identification label Inlet port
Underside of device 66801791
O-ring 9
Barcode label
EN
Device orientation during use The device is designed to operate in the upright position. Device orientation, rate at which fluid enters the canister and how exudate solidifies can impact filter occlusion. Operation in the upright position optimizes canister volume and alarm functionality. The device should be orientated to face the user's position when in stationary use. Proper use/correct orientation The 300ml canister has a kickstand and rubber feet. The device can stand in the upright position with the 300ml canister attached. Open the kickstand for additional stability and to change the viewing angle. The 800ml canister does not include a kickstand or rubber feet. The IV pole/bed clamp or carry strap accessories can be used to mount the device in the upright position.
300ml canisters only
300ml or 800ml canisters with clamp
300ml or 800ml canisters with carry strap
Incorrect orientation Caution: Operating the device in a face-down position could result in damage to the device and inadvertent changes to therapy settings. Operating the device in an inverted position could impact filter occlusion resulting in a blockage alarm and requiring a change of canister.
300ml or 800ml canisters
300ml or 800ml canisters
10
EN
Dressing changes
Canister selection
1. Foam dressings should be changed every 48 to
Only use Smith & Nephew RENASYS™ TOUCH canisters with the RENASYS TOUCH device.
72 hours after the initial application of therapy. If no leak is present and the patient is comfortable, dressing changes should occur no less than 3 times per week.
RENASYS TOUCH canisters use an integral two stage bacterial filter for protection of the device against overflow and the spread of aspirated micro-organisms.
2. Gauze dressings should be changed 48 hours
Canisters are designed for single patient use. DO NOT REUSE. Use of the canisters on more than one patient may result in cross contamination that may lead to infection.
3. In the event of heavy drainage, drainage with
Canisters should be changed at least once a week, whenever there is a change of patient, or when the contents reach the maximum volume indication (300ml or 800ml fill line) in the viewing window. Do not wait for the Canister Full alarm to sound to change canister.
after the initial application of therapy. If no leak is present and the patient is comfortable, dressing changes should occur 2-3 times per week.
sediment, or when blood is present, regular monitoring and more frequent dressing changes may be required.
4. When dressing a wound involving difficult to seal
anatomy or exposure to external moisture, frequent inspection of the dressing is recommended to ensure a seal is maintained. Ensure wound dressing is fully sealed and firm to the touch.
For patients with high risk of bleeding, use the 300ml canister. Canisters may have to be changed regularly within single patient treatments if exudate levels are high. Check canisters regularly to monitor exudate levels, ensuring they are below the canister maximum volume indication.
5. Ensure all wound filler material placed in the
wound has been removed before redressing the wound. If foam dressing adheres to the wound, apply normal saline into the wound dressing and wait for 15-30 minutes before gently removing the foam. Appropriately discard used wound dressings observing your institution’s protocol for medical waste handling.
Canisters are non-sterile and should not be used in a sterile field. Note: Check canister for any signs of cracks or damage. If noted, discard and replace canister. Note: Change or replace canisters that have been dropped or mishandled even if no visible signs of damage are present to ensure correct operation of software alarms for leak and blockage.
6. As with all adhesive products, apply and remove
the dressing carefully from sensitive or fragile skin to avoid skin stripping, especially after frequent dressing changes. Use of skin sealant may assist with protection of periwound skin.
7. Check the dressing regularly. Monitor the patient
for any signs of local or systemic infection. Infected wounds may require more frequent dressing changes. If there are any signs of systemic infection or advancing infection at the wounded area, contact the treating clinician immediately.
300ml canister
8. Sealed dressings should be firm to the touch and leak free while therapy is active.
Canister Viewing window
Canister clip Rubber feet
Kickstand Canister tubing
800ml canister
Quick click connectors with tethered caps
11
EN
Installing canister 1. Ensure therapy is paused or device is Off. 2. Remove paper tape around canister tubing and release tubing to full length.
3. Open canister clips on both sides of the canister. 4. Position the canister so that the viewing window is facing forward.
300ml and 800ml canisters
5. Push canister gently over inlet port on the bottom of the device.
6. Engage both canister clips. Canister clips will click when properly engaged.
7. Connect the dressing to the canister tubing by
pushing quick click connectors together. Quick click connectors will click when properly engaged.
Note: Do not cover the aeration disc for proper delivery of therapy.
Removing/changing canister 1. Pause therapy or turn device Off. 2. Hold the quick click connectors above the level of the
wound to ensure exudate does not leak from the tubing.
3. Disconnect canister tubing from dressing tubing by applying pressure to the canister quick click connector and gently pulling connectors apart.
4. Close the tethered caps of both quick click
connectors to protect both sides of tubing and prevent leakage.
5. Release canister clips on both sides of device and gently pull canister away from device.
300ml or 800ml canisters
Disposal of used canisters should follow facility protocols or local ordinances relating to handling of potentially infected or bio-hazardous materials.
12
EN
Turning on device Ensure the battery is fully charged if battery operation is required for first use of the device. Press and hold the Power
button below the touchscreen for 2 seconds to power On (or power Off) the device.
The touchscreen illuminates and initiates the start up sequence: the Smith & Nephew start up screen will display, the status indicator will flash yellow then green, the device sounds an audible tone, then the Welcome screen will display. The Home screen will display upon completion of the start up sequence.
*smith&nephew
Note: When the device is nearing time for the annual maintenance check, an annual maintenance notification will display when powering On the device. To close this notification screen and continue to the Home screen, press the Accept icon.
Navigating the touchscreen interface The screen on the RENASYS™ TOUCH device is touch sensitive. Tap the touchscreen to make a selection. Slide your finger up, down or across the screen to scroll. Note: The touchscreen should only be actuated by finger. Using pens or other pointed objects may damage the screen Home screen (Continuous therapy mode shown)
Status indicator
Therapy set point
GPS 3G indicator
Date & Time Indicators
Battery indicator Alarm volume indicator
Settings
Therapy indicator
Log Decrease value Increase value Help Therapy mode toggle 13
Y-Connect toggle
EN
Setting therapy
Caution: Due to its smaller diameter, the RENASYS-G 10 Fr Round Drain Gauze Kit and Accessory Kit are not recommended for use with RENASYS TOUCH, as reduced pressure in the wound bed may lead to pooling or maceration.
The prescribed therapy setting is a decision that the clinician must make based on an assessment of the particular wound. These general guidelines should be adhered to: •
40–120mmHg is the recommended therapeutic pressure range.
•
NPWT should never be painful. If the patient reports discomfort, consider reducing the pressure setting.
•
Outside the recommended optimal therapeutic pressure range of 40 – 120mmHg, the broader operating range of 25 – 200mmHg is provided to support clinical discretion on pressure set-point.
Set therapy mode The device features two therapy modes: Continuous and Intermittent. Press the Therapy Mode toggle icon to switch between Continuous and Intermittent therapy. Note: Therapy must be paused to change therapy mode. Continuous therapy mode In Continuous mode, the device will maintain the selected therapy level until therapy is stopped or changed. The therapy set point is displayed in the center of the screen. Therapy levels can be selected from a range of 25–200mmHg by pressing the Decrease and Increase icons.
The device will display the therapy set point. Set Y-Connect Select Y-Connect On to adjust the blockage alarm to account for two dressings connected to the device. Select Y-Connect Off if only one dressing is connected to the device. Press the Y-Connect toggle icon to switch between Y-Connect Off and Y-Connect On . Press the Accept icon to confirm your selection.
Press the Cancel setting.
(Continuous therapy mode shown) Therapy set point
icon to maintain the current
Decrease value Therapy mode toggle
Note: Therapy must be paused to change Y-Connect setting. This feature is unavailable in Patient Mode Caution: The system will only detect a blockage if both connections are blocked. The system will not detect a blockage existing in one of the Y-connected dressings; therapy will not be delivered through the blocked dressing. Setting Y-Connect On when only one dressing is connected to the device may cause nuisance alarms. Setting Y-Connect Off when two dressings are connected to the device may prevent blockage alarm from sounding. 14
Increase value Y-Connect toggle
EN Intermittent therapy mode Enter information into the fields shown on the screens.
Intermittent therapy mode provides both intermittent and variable therapy set point options. The device will alternate between set points of active therapy and low (variable) or no (intermittent) therapy at set cycle times.
To cancel press the Home
icon.
To adjust the therapy set points and cycle times: 1.
Select to highlight the setting that needs adjustment.
2. Press the Decrease or Increase icon to select therapy set points and cycle times with the following range.
Shrink Keyboard using the information has been put in.
• High therapy: 25–200mmHg
icon when all
• Low therapy: 0–180mmHg (will not equal or exceed High therapy) • High cycle time: 3,5,8,10 minutes Low cycle time: 2,3,5,8,10 minutes Intermittent therapy is not recommended for: • Highly exuding wounds Press “Start/Resume Usage” Icon to start therapy.
• Wounds with tunnels or undermining • Wounds in difficult areas where maintaining a seal is problematic • Patients who experience pain during intermittent therapy Note: Therapy must be paused to change cycle times. (Intermittent therapy mode shown) High therapy
As the device begins delivering therapy, it will perform a leak check to determine if the system is sealed or if there is a significant leak in the system.
High cycle time
(Intermittent therapy mode shown) Leak Check
Low therapy
Low cycle time Seal Achieved
Starting therapy Before starting therapy, check that the prescribed therapy settings have been properly set. Caution: Ensure the device and system tubing are positioned level with or below the wound and are away from any direct sources of heat. Press the Start/Pause Therapy touchscreen.
button below the
15
EN Delivering Therapy
Press the icon to confirm you want to end therapy.
Active Therapy Set Point Active Cycle Time Next Therapy Set Point and Cycle Time
When therapy is active, the therapy indicator at the top of the screen will rotate orange and status indicator on top of the device illuminates green.
If you wish for the Device to be collected, tick Yes and enter the information into the fields.
If a significant leak is detected in the system, the device will indicate a leak alarm. Refer to "Alarms/ Troubleshooting" section for more details.
Confirm your selection by pressing the
icon.
To return to Home screen while therapy is active, press the Home icon on the Delivering Therapy screen. After 10 seconds without user interaction, the touchscreen will automatically return to the Delivering Therapy screen. If you have navigated to the Help menu or the Flow Meter within the Settings menu, the touchscreen will automatically return to the Delivering Therapy screen after 3 minutes without user interaction.
When complete, the touchscreen will return to the Home screen.
Pause therapy
Lock/Unlock feature
Therapy may be paused by pressing the Start/Pause Therapy button.
To lock the user interface when therapy is active, press and hold Lock/Unlock button below the touchscreen for 2 seconds. Once locked, a lock symbol will appear behind the therapy set point and the device will enter Sleep mode.
When paused the touchscreen will give options to Resume or End Usage. Press “Start/Resume Usage” Icon to continue therapy or “End Usage” icon to end therapy.
While in Sleep mode, the touchscreen will go dark for user comfort and to conserve battery life. The status indicator continues to illuminate green to indicate the device is delivering therapy. In the event of an alarm, the device will automatically unlock and the alarm screen will display. The device will automatically Lock and enter Sleep mode after 5 minutes without user interaction when To unlock user interface, press and hold the Lock/Unlock button for 2 seconds.
End Therapy To end therapy, pause therapy (as per the Pause Therapy section above.) Press ‘End Usage’ button.
16
EN
Settings Settings contains a menu of user preferences, device functions and device information. Scroll up and down to view all selections.
Note: Therapy must be paused to change Compression Rate. Change mode The device has three user modes: Clinician Patient and Maintenance .
,
Clinician Mode provides healthcare professionals full access to features and settings. Patient Mode prevents inadvertent changes to therapy settings by restricting access to the following features:
Alarm volume Select Alarm Volume from the Settings menu and choose low, medium or high to adjust alarm volume. The device will issue a sample tone as you make your selection. Alarm volume indicators on the Settings menu and at the top of screen will update based on the selection.
•
Therapy settings: therapy set points, cycle times, therapy mode and Y-connect selection will display on the touchscreen but cannot be changed.
•
Settings menu selections: Restore Presets and 3G and GPS will display in the settings menu but cannot be selected.
Maintenance Mode allows authorized service personnel access to reset the Annual Maintenance timer. Refer to "Annual Maintenance" section under "Alarms/Troubleshooting" section for details. To switch between modes, select Change Mode from the Settings menu and choose Clinician or Patient.
Compression rate The compression rate limits the target pressure change in a given period of time to a maximum amount. Selecting the high compression rate will result in the most rapid dressing draw down. Select Compression Rate from the Settings menu and choose low, medium or high. The Compression Rate indicator on the Settings menu will update based on the selection.
A password is required to switch between Clinician and Patient modes. Enter the numeric password (3141) and press the Accept icon.
17
EN To delete a number that was entered incorrectly, press the Back icon. To exit the screen without entering a password, press the Cancel icon.
Time zone Select Time Zone from the Settings menu and choose desired time zone from the available list to change the displayed date and time at the top of the touchscreen.
Note: Patient Mode restricts access to therapy settings and specific device features. It is recommended that clinicians set the device to Patient Mode once therapy settings have been selected to prevent inadvertent changes to settings.
Flow meter The Flow Meter provides a visual indication of the rate of air flow in the system to help determine if the system is properly sealed or if there are leaks. The gauge will turn yellow if a significant leak is detected. To access the Flow Meter, select Flow Meter from the Settings menu.
Language To change the language, select Language from the Settings menu and choose desired language from provided list. Scroll up and down to view all selections.
In the event of a leak alarm, the Flow Meter is displayed on the alarm screen to assist in locating leaks in the system.
Set Date and Time Select Set Date and Time from the Settings menu. 1. Select to highlight the setting that needs adjustment. 2. Press the decrease change the time or date.
or increase
Confirm your selection by pressing the
icon to icon.
Send data The RENASYS TOUCH device contains integrated global cellular technology that allows device location, billing and maintenance data to be sent to a secure Internet website. The device will transmit data every hour if the 3G and GPS setting is Enabled, the device is connected to the cellular network and the device is connected to AC mains power. The device will transmit data every two hours while running on battery power. The device must be powered on to transmit data.
18
EN
It is recommended to manually initiate a data transmission at the conclusion of a patient’s therapy and before selecting Restore Presents in the Settings menu to ensure device data is communicated. To manually initiate a data transmission:
1. Ensure 3G and GPS setting within the Settings menu is enabled.
Note: This feature is unavailable if 3G and GPS are turned off. Refer to 3G and GPS under the Settings.
2. Ensure adequate signal strength by checking the GPS 3G status indicator at the top of the screen.
Restore presets
3. Select Send Data from the Settings Menu.
Restore Presets should be selected whenever the device is prepared for use with a new patient.
4. Press Accept
icon to initiate data transmission or Cancel icon to cancel and return to the Settings Menu.
Select Restore Presets from the Settings menu and press Accept icon to restore the device to the factory presets below: •
The screen will display the status of the transmission and then return to the Settings menu once the transmission is complete.
All Log information is reset to zero.
•
Continuous Therapy: 80mmHg
•
Intermittent Therapy: 80mmHg for 5 minutes; 0mmHg for 2 minutes
•
Y-Connect: Off
•
Compression rate: High
•
3G GPS: Enabled
•
Alarm volume: High
Press the Cancel settings.
icon to maintain the current
Note: This feature is unavailable in Patient mode. 3G and GPS
If the transmission fails, the screen will display a Data Not Sent notification.
Press the Cancel screen.
The RENASYS TOUCH device contains integrated global cellular technology that allows device location, billing and maintenance data to be sent to a secure Internet website. The device will transmit data every hour when the 3G and GPS are Enabled, the device is connected to the cellular network and the unit is connected to AC mains power. The device must be powered On to transmit data.
icon to return to the Send Data
When the 3G and GPS are Disabled the device will not transmit data and Send Data in the Settings menu cannot be selected to manually initiate a data transmission. To turn on or off the 3G and GPS, select 3G and GPS from the Settings menu and select Enabled to turn on or Disabled to turn off the functionality. 19
EN
Note: Format is Days, Hours, Minutes.
Note: This feature is unavailable in Patient mode. Device Information
Help
To display a list of device information, such as serial number, battery charge remaining, software information and annual maintenance timing, select Device Information from the Settings menu to view.
The Help menu provides guidance on device functions and operation, troubleshooting assistance, Smith & Nephew contact information, and licensing details. Scroll up and down to view all selections.
Alarms/Troubleshooting Descriptions of each alarm are provided with step-by-step instructions to assist in resolving the alarms. Select Alarms/Troubleshooting from the Help menu and scroll up and down to view all menu selections. Select the alarm you would like assistance with and scroll up and down to view the instruction steps.
Pump Activity Log The Pump Activity Log displays total pump activity since reset (accumulated active days, hours and minutes since last Restore Presets) and provides information on pump activity that may have been delivered to the patient in two display formats: Overview and Detailed view. Select the Log toggle icon to switch between Overview and Detailed view. Overview displays a bar graph of total pump activity hours per day. Scroll left or right to view additional days.
Detailed view displays a history of events, including therapy settings, alarms and device status. Scroll up and down to view additional days.
20