4WEB
16 x 14 x 4.5 mm COTS Implant, Osteotomy Truss System
Osteotomy Truss System (OTS) Instructions for Use
1 Page
Preview
Page 1
The instruments used to implant the OTS devices do not have an indefinite functional life. All reusable instruments are subjected to repeated stresses related to bone contact, impaction and routing, cleaning, and sterilization processes. Instruments should be carefully inspected before use to ensure that they are fully functional. OSTEOTOMY TRUSS SYSTEM (OTS) INSTRUCTIONS FOR USE PLEASE READ CAREFULLY CAUTION: FEDERAL LAW (USA) RESTRICTS THESE DEVICES TO SALES BY OR ON THE ORDER OF A PHYSICIAN. INTENDED USE: The Osteotomy Truss System (OTS) implants are intended to provide stability and facilitate fixation of bones of the foot. DEVICE DESCRIPTION: The device is an open architecture truss design mathematically formulated to provide structural support with open space throughout the implant for bone growth and fixation. The 4WEB additive manufacturing process provides a hierarchical surface roughness. The implant is made from Ti6Al4V alloy. The device is available in a variety of sizes and angles to accommodate the patient’s anatomy. INDICATIONS FOR USE: The Osteotomy Truss System (OTS) is intended to be used for internal bone fixation for bone fractures or osteotomies in the foot, such as: • Opening wedge osteotomies of the bones of the foot including osteotomies for Hallux Valgus • Opening wedge of Medial Cuneiform or Cotton osteotomies • Lateral Column Lengthening (Evans Lengthening Osteotomy or Calcaneal Z Osteotomy) • Metatarsal/Cuneiform osteotomies • Nonunion of arthrodesis of the Midfoot including Metatarsal/Cuneiform osteotomies (TMT or Lapidus) • Hindfoot osteotomies The device is intended for use with supplemental fixation. The Osteotomy Truss System is not intended for use in the spine. CONTRAINDICATIONS: The OTS devices should not be implanted in patients with: • Active infection at the operative site or other active systemic infection • Inadequate physiological or psychological condition • Inadequate skin, bone, or neurovascular status • Irreparable tendon system • Growing patient with open epiphyses • Known sensitivity to the material WARNINGS AND PRECAUTIONS: Safety and effectiveness have not been established in the following conditions: • Gross obesity • Previous fusion attempts at the osteotomy/fusion site • Significant loss of bone stock as seen with osteoporosis or osteomalacia • Conditions requiring chronic corticosteroid use • Active drug abuse The OTS devices are for single use only. Bending or fracture of the implants or instruments can occur if not handled properly. All implants and instrumentation are provided non-sterile and must be steam sterilized prior to use. No implant should be reused if it has come in contact with blood or other bodily fluids. All implants, sizers and instrumentation should be inspected prior to use for possible damage or defects. Any damaged or defective component should not be used and should be returned to 4WEB. The OTS devices are intended to provide mechanical support while biologic fusion occurs. In the event of pseudoarthrosis or delayed fusion, the risk of implant migration, loosening or breakage increases. The physician/surgeon should consider patient weight, patient activity level, other patient conditions, etc. which may impact the performance of the system. Patients requiring abnormal or excessive forces on the implanted area may not be good candidates for this type of surgery. Do not attach supplemental fixation hardware to or through the OTS device. In patients with a high level of activity, the benefits must be weighed against possible risks. The correct implant size must be selected to provide adequate bone support. All OTS devices must be used with ancillary fixation. These should be compression plates made from a compatible titanium alloy and not bioresorbable. OPERATIVE PRECAUTIONS: The surgeon is to be thoroughly familiar with the OTS devices, method of application, instruments and surgical technique. Correct positioning of the OTS device should be checked intraoperatively with x-ray. The size (and more particularly the height) of the OTS device must be chosen on the basis of the patient’s anatomy and desired correction. The implants are for single-implant use only. An explanted implant must never be re-implanted. Stresses and fracture, even though not noticeable by visual inspection, may have been created during initial implantation. Following implantation, the product number and manufacturing serial number of the device that has been implanted must be reported in the patient’s surgical file. POTENTIAL ADVERSE EVENTS: Potential adverse events may be related to any surgery in general, foot surgery specifically, or to the device. These may include, but are not limited to the following: • Adverse events related to any surgery: reactions to anesthesia, the anesthetic or other medications, infection, ileus, atelectasis, pneumonia, urologic problems, anemia, heart attack, stroke or death. • Adverse events related specifically to foot surgery: bleeding, blood vessel damage, nerve or soft tissue damage, hematoma, seroma, wound dehiscence or incisional hernia, embolism, or thrombophlebitis. • Adverse events related to the device: implant crack or fracture, failure to achieve fusion, implant migration, dislodgement, or metal sensitivity to a foreign body, including possible tumor formation. Additional surgery may be necessary for implant removal, repositioning or replacement. POSTOPERATIVE CARE: The physician’s postoperative directions and warnings to the patient and the corresponding patient compliance are extremely important. • Detailed instructions on the use and limitations of the device must be given to the patient. The patient must be warned that loosening, and/or breakage of the device(s) are complications which may occur as result of early or excessive weight-bearing, muscular activity or sudden jolts or shock to the foot. • The patient must be advised not to smoke or consume alcohol during period of the bone fusion process. • The patient must be advised of the inability to bend at the point of osteotomy or fusion and taught to compensate for this permanent physical restriction in body motion. • It is critical that immobilization of union is established and confirmed by roentgenographic examination. If a non-union develops or if the components loosen, migrate, and / or break, the devices must be revised and/or removed immediately before serious injury occurs. • Any retrieved devices are not to be used in another surgical procedure. MRI SAFETY INFORMATION: Non-clinical testing has demonstrated the OTS device is MR Conditional. A patient with this device can be safely scanned in an MR system meeting the following conditions: • Static magnetic field of 3 T or 1.5 T • Maximum spatial field gradient of 1900 gauss/cm (19 T/m) • Maximum MR system reported, whole body averaged specific absorption rate (SAR) of ≤ 2 W/kg (Normal Operating Mode)
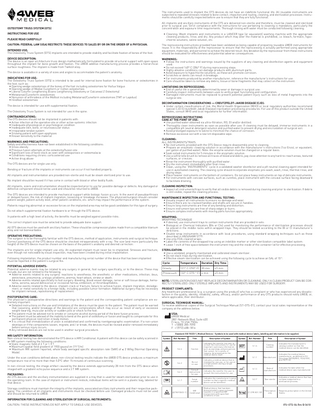
All implants and ancillary instruments of the OTS are delivered non-sterile and therefore, must be cleaned and sterilized prior to surgical use. Strict compliance with the instructions for use pertaining to cleaning is mandatory, particularly the concentration and exposure time requirements. Thorough rinsing with water must be conducted following cleaning. • Cleaning: Wash implants and instruments in a LANCER type (or equivalent) washing machine with the appropriate cleaning products, rinse, and dry. Any product which may alter the material is prohibited, i.e. bleach, formalin, hypochlorite solutions, saline solution, etc. The reprocessing instructions provided have been validated as being capable of preparing reusable 4WEB instruments for reuse. It is the responsibility of the reprocessor to ensure that the reprocessing is actually performed using appropriate equipment, materials, and personnel to achieve the desired result. Any deviation by the reprocessor from these instructions should be evaluated for effectiveness and potential adverse consequences. WARNINGS: • Follow the instructions and warnings issued by the suppliers of any cleaning and disinfection agents and equipment used. • Do not exceed 140º C (284º F) during reprocessing steps. • Highly alkaline conditions can damage products with aluminum parts. • Avoid exposure to hypochlorite solutions, as these will promote corrosion. • Scratches or dents can result in breakage. • For instruments produced by another manufacturer, reference the manufacturer’s instructions for use. • Care should be taken to remove any debris, tissue or bone fragments that may collect on the instrument. LIMITATIONS ON REPROCESSING: • End of useful life is generally determined by wear or damage in surgical use. • Carefully inspect instruments between uses to verify proper functioning and configuration. • Damaged instruments must be replaced to prevent potential patient injury such as loss of metal fragments into the surgical site. DECONTAMINATION CONSIDERATIONS - CREUTZFELDT-JAKOB DISEASE (CJD): • Under certain classifications of risk, the World Health Organization (WHO) or local regulatory authorities recommend special CJD (Creutzfeldt-Jakob Disease) inactivation processing procedures. For use of this product outside the United States, consult WHO and local regulations for further information. REPROCESSING INSTRUCTIONS CARE AT THE POINT OF USE: • Use purified water obtained via ultra-filtration, RO, DI and/or distilled. • Thoroughly clean instruments as soon as possible after use. If cleaning must be delayed, immerse instruments in a compatible pH neutral detergent solution and purified water to prevent drying and encrustation of surgical soil. • Avoid prolonged exposure to saline to minimize the chance of corrosion. • Remove excessive soil with a low lint disposable wipe. CLEANING: ALL INSTRUMENTS/TRAYS • No instruments provided with the OTS Device require disassembly prior to cleaning. • Prepare an enzymatic cleaning solution in accordance with the manufacturer’s instructions (1oz Enzol, or equivalent, per gallon of purified water). Note: the enzyme solution must be changed on a regular basis. • Soak soiled instruments for 5 minutes in the enzymatic solution. • Use a soft bristle brush to remove all traces of blood and debris; pay close attention to any hard-to-reach areas, textured surfaces, or crevices. • Rinse the instrument thoroughly with purified water. • Dry the instrument immediately after final rinse. • Clean, using the “INSTRUMENTS” cycle in a validated washer disinfector and a pH neutral cleaning agent intended for use in automated cleaning. The cleaning cycle should incorporate enzymatic pre-wash, wash, rinse, thermal rinse, and drying steps. • Place heavier instruments on the bottom of containers. Do not place heavy instruments on top of delicate instruments. • For instruments with concave surfaces, such as curettes, place instrument with the concave surface facing downward to facilitate draining. CLEANING INSPECTION: • Inspect all instruments/trays to verify that all visible debris is removed during cleaning and prior to sterilization. If debris is still visible, repeat the cleaning process. MAINTENANCE INSPECTION AND FUNCTIONAL TESTING: • Visually inspect all instruments to ensure no damage and wear. • Ensure there are no cracked handles and shafts are secure in handles. • Ensure long instruments are free of any bending and distortion. • Ensure instrument tips are free of sharp edges or burrs. • Ensure complex instruments with moving parts function appropriately. WRAPPING: WRAPPING TECHNIQUE • If desired, use instrument trays to contain instruments that are provided in sets. • Biological or Chemical Indicators (BIs or CIs) used for monitoring the performance of sterilization processes should be placed in the middle racks within wrapped trays. They should be tested according to the BI or CI manufacturer’s directions. • Double wrap instruments in accordance with local procedures, using standard wrapping techniques such as those described in ANSI/AAMI ST79. • Use only FDA-cleared wraps. • Label the contents of the wrapped tray using an indelible marker or other sterilization compatible label system. • Leave 1 inch of free space between the instrument tray and the inside of the container lid for effective processing. STERILIZATION: • Use a validated, properly maintained and calibrated steam sterilizer. • Do not stack trays during sterilization. • Effective steam sterilization can be achieved using the following cycle to achieve an SAL of 10-6. Cycle
Temperature
Gravity
121° C (250° F) 30 min
45 min
Prevacuum
132° C (270 ° F) 4 min
45 min
NOTE: STERILIZATION DOES NOT REPLACE DECONTAMINATION OR CLEANING. ONLY A CLEAN PRODUCT CAN BE CORRECTLY STERILIZED. ONLY STERILE IMPLANTS AND INSTRUMENTS MAY BE USED FOR SURGERY. PRODUCT COMPLAINTS: Any healthcare professional (e.g. a surgeon using the product) who has a complaint or who has experienced any dissatisfaction in the quality, identity, reliability, safety, efficacy, and/or performance of any OTS products should notify 4WEB, or, where applicable, their distributor. SURGICAL TECHNIQUE MANUAL: To receive additional copies of the Surgical Technique Manual (ST-OTS-01), contact your local sales representative or the company at the address below. USA: 4WEB Medical 2801 Network Blvd. Suite 620 Frisco, TX USA 75034 T +1(800) 285-7090 F +1(972) 488-1816 Standard: ISO 15223-1, Medical Devices - Symbols to be used with medical device labels, labelling and information to be supplied. Symbol
Ref. Number
Storage conditions must maintain the integrity of the implants, associated ancillary instruments and their respective packaging. The condition of all implants and instruments must be checked before use. Damaged products must not be used and should be returned to 4WEB.
SN
Title
Description of Symbol
5.1.6
Catalog number
Indicates the manufacturer’s catalog number so that the medical device can be identified.
5.1.1
Manufacturer
Indicates the medical device manufacturer, as defined in EU Directives 90/385/EEC, 93/42 EEC, and 98/79 EC.
5.1.3
Date of manufacture
Indicates the date when the medical device was manufactured.
Indicates the manufacturer’s serial number so that a specific medical device can be identified.
5.2.7
Non-sterile
Indicates a medical device that has not been subjected to a sterilization process.
Medical device that has been demonstrated to pose no known hazards in a specified MR environment with specified conditions of use.
21 CFR 801.109
Prescription only
Requires prescription in the United States.
Description of Symbol
Caution
Indicates the need for the user to consult the instructions for use for important cautionary information such as warnings and precautions that cannot, for a variety of reasons, be presented on the medical device itself.
5.4.2
Do not re-use
Indicates a medical device that is intended for one use, or for use on a single patient during a single procedure.
5.4.3
Consult instructions for use
Indicates the need for the user to consult the instructions for use.
5.1.7
Serial number
ASTM F2503-13
MR Conditional
In non-clinical testing, the image artifact caused by the device extends approximately 28 mm from the OTS device when imaged with a gradient echo pulse sequence and a 3 T MR system.
Symbol
Ref. Number
Title
5.4.4
Under the scan conditions defined above, non-clinical testing results indicate the 4WEB OTS device produces a maximum temperature rise of no more than than 5.0°C after 15 minutes of continuous scanning.
PACKAGING: All OTS devices and the ancillary instrumentation are supplied in a tray that is used for steam sterilization prior to use in the operating room. In the case of implant or instrument restock, individual items will be sent in a plastic bag, labeled for that device.
Duration Dry Time
INFORMATION FOR CLEANING AND STERILIZATION OF SURGICAL INSTRUMENTS: CAUTION: THESE INSTRUCTIONS DO NOT APPLY TO SINGLE-USE DEVICES.
IFU-OTS-04 Rev B 0618