Moller Medical
Handgrip for manual liposuction
Reprocessing instruction for reusable liposuction cannulas from Möller Medical
16 Pages
Preview
Page 1
Liposuction cannulas
en
Reprocessing instruction for reusable liposuction cannulas from Möller Medical
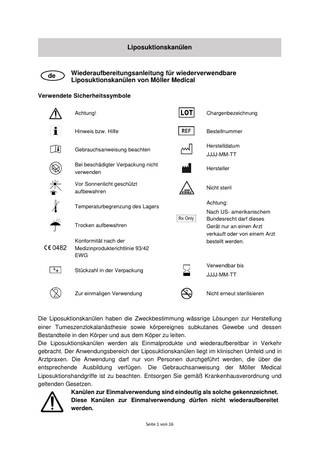
Symbols used Caution!
Batch code
Information or help
Catalogue number Date of manufacture
Consult instructions for use
YYYY-MM-DD Do not use if package is damaged
Manufacturer
Keep away from sunlight
Non-sterile
Storage temperature limitation
Attention:
Keep dry
Conformity with Medical Device Directive EEC 93/42
Under US federal law, this device may be only sold to a physician or ordered by a physician. Use by
Unit quantity in packaging
YYYY-MM-DD
Do not reuse
Do not resterilise
The intended use of the liposuction cannulas is to pass aqueous solutions for the production of tumescent local anesthesia as well as subcutaneous body tissue and its components into the body and out of the body. The liposuction cannulas are placed on the market as single-use products and as reusable. The scope of application of liposuction cannulas falls within the clinical environment and in medical practices. The application may only be carried out by persons who have the appropriate training. The instructions for use of the Möller Medical liposuction hand pieces must be observed. Dispose of in accordance with hospital regulations and applicable laws.
Needles for single-use are clearly labelled as such. These cannulas for single-use must not be reused.
page 9 to 16
General principles and information Clean, disinfect and sterilize all cannulas prior to use. All cannulas are not sterile upon delivery. (Cleaning and disinfection after removal of the protective transport packaging; sterilization after packaging). Effective cleaning and disinfection are a prerequisite for effective sterilization. Within the scope of your responsibility, ensure that the cannulas are sterile prior to use: •
Only cleaning/disinfection and sterilization procedures which have been sufficiently validated for the device and product must be employed.
•
The devices used (washer and disinfector, autoclave) must be maintained and tested regularly.
•
The validated parameters must be observed during each cycle.
When selecting the washer/disinfector, it must be ensured that •
the effectiveness of the washer/disinfector has been tested (e.g. DGHM or FDA approval/clearance/registration or CE marking as per DIN EN ISO 15883),
•
as far as possible a tested program for thermal disinfection (A0 value > 3000 or – for older devices – at least 5 min. at 90°C/194°F) is used (with chemical disinfection there is a risk of disinfection residue on the instruments),
•
the program used is suitable for the cannulas and contains sufficient rinsing cycles,
•
only sterile or low-germ (max. 10 germs/ml) or low-endotoxin (max. 0.25 endotoxins/ml) water (e.g. purified water/highly purified water) is used for rinsing,
•
the air used for drying is filtered (oil-free, low-germ, low-particle),
•
the chemicals used are compatible with the instruments (see chapter “Material resistance”).
Observe the instructions issued by the manufacturer of the cleaning and disinfection agents in terms of concentration, temperature, exposure time and details on rinsing. Only freshly produced solutions, sterile or low-germ (max. 10 germs/ml) or low-endotoxin (max. 0.25 endotoxins/ml) water (e.g. purified water/highly purified water) may be used. Soft, clean and lint-free cloths or filtered air are to be used for drying. Also observe the valid legal provisions in your country as well as the hygiene regulations of the doctor’s practice or hospital. This applies in particular to the various specification as regards effective prion inactivation.
After the treatment of a patient infected with Creutzfeldt-Jakob disease, the cannulas must not be reused or reprocessed. The cannulas must be disposed of! Sterilization devices offer different configurations and capacities. Check whether the cycle parameters of your sterilizer correspond to the parameters in the sterilization instructions included in this manual.
page 10 to 16
Only use cleaning solutions with a mild pH value. Do not use cleaning agents containing chlorine or chloride, as the active ingredient damage stainless steel. Follow all cleaning steps that are included in this manual to achieve the required cleanliness and sterility of the products.
Restrictions on reprocessing Reusability Frequent reprocessing has little effect on these cannulas. The end of the product life is normally determined by wear and damage due to use. Check all cannulas for damage and wear before each use. If cracks, corrosion or deformation of the cannulas are detected or the socket is defective, the cannula must not be used any further. Cleaning and disinfection Basics For an optimal cleaning and disinfection result an automatic process (RDG (cleaning and disinfection device)) must be in charge. 1. Cleaning Immediate cleaning at the place of use Cannula cleaning and reprocessing must start within 30 minutes after the use of the cannula in the surgical case. Remove visible soil contamination from the cannulas immediately after use with a disposable cloth and cover the products with a cloth moistened with demineralized water. Do not use water with a temperature > 40 °C (104 °F) or other fixative agents, as this can lead to residues adhering to the product and thus impair the cleaning performance of the subsequent cleaning. Manual cleaning/precleaning a. Immerse the cannulas for 5 minutes in cold, demineralized water with a suitable
cleaning agent (e.g. Incidin Plus) and make sure that the cannulas do not touch each other. In order to avoid this, we recommend to swivel the cannulas slightly in the water bath. Actuate the cannula connection lock several times. b. Brush the outside surface for at least 30 seconds immediately after withdrawal, until
all visible contaminants have been removed. For this purpose, use a cleaning brush with plastic bristles. Wipe down the outside surface with manual force for 30 seconds using a lint-free cloth. Rinse the interior lumen of the cannula and the socket using the water pistol or syringe for at least 10 seconds. Clean the interior lumen of the cannulas using a suitable inner brush (e.g. Möller Medical cleaning brush for inner lumen). For this purpose, insert the brush into the proximal opening (socket side) and turn it twice around its own longitudinal axis. Then pull the brush out. Repeat the cleaning of the interior lumen at least twice until page 11 to 16
there are no visible soils. If soils become visible during cleaning, it must be rinsed off. Rinse the interior lumen and the socket using a water pistol or syringe for at least another 10 seconds and then brush again. When cleaning, safety equipment including protective goggles and masks (PPE) must be worn to prevent contamination. c. Then rinse the cannulas under running, demineralized water < 40 °C / 104 °F for
30 seconds. Hold the cannula socket upwards so that the water drains through the tip of the cannula. d. Place the cannulas on instrument carriers so that they do not touch each other (to
avoid acoustic and spray shadow). e. Immerse the cannulas at 40 °C for 15 minutes in an ultrasonic bath with e.g. Incidin
Plus and activate it. f. Remove the cannulas and rinse them through and off with cold water. g. If visible contamination remains, repeat steps a-f.
Automatic cleaning a. After pre-cleaning, adapt the cannulas to the rinsing sleeves in the upper basket of
your washer/disinfector (e.g. Miele G7882 with upper basket O183 and rinsing sleeve E442). b. Start the program. c. Remove the cannulas from the washer/disinfector at the end of the program. d. As far as possible, check and pack the cannulas immediately after removal from
the washer/disinfector (see chapters “Checking”, “Maintenance” and “Packaging”, if necessary, after additional drying in a clean place). The following cycle in the rinsing/disinfection machine is recommended as a minimum: Proof of the fundamental suitability of instruments for effective manual cleaning and disinfection was provided by an independent, officially accredited and recognized (Section 15 (5) German Medical Devices Act) testing laboratory using the washer/disinfector G 7836 CD (thermal disinfection, Miele & Cie. GmbH & Co., Gütersloh) and precleaning and cleaning agent Neodisher MediZym (Dr. Weigert GmbH & Co. KG, Hamburg). The procedure described above was taken into consideration.
#
Designation
Cleaning agents
Minutes
Temp.
1
Precleaning
Cold water
4
< = 50 °C (122 °F)
2
Main cleaning
e.g. Neodisher Medizym
10
~ 55 °C (131 °F)
3
Neutralization
e.g. Neodisher Z
6
< = 50 °C (122 °F)
4
Intermediate rinsing
Cold water
3
< = 50 °C (122 °F)
5
Thermal disinfection
Without
5
90 - 95 °C (140 °F)
6
Post rinsing
Cold water
5
< = 50 °C (122 °F)
7
Drying
Without
35
> = 99 °C (210 °F)
The rinsing/disinfection machine must satisfy the requirements of the standard ISO 15883. It must be properly installed and checked regularly as per ISO 15883.
page 12 to 16
2. Disinfection manual •
Place the cleaned and checked cannulas in the disinfection bath for the specified exposure time, making sure they are properly covered. The cannulas must not touch each other.
•
Remove the cannulas from the disinfection bath and rinse these through and off with water at least five times (min. 1 minute). Dry the cannulas by blowing out and through with filtered compressed air.
•
As far as possible, pack the cannulas immediately after removal (see chapter “Packaging”, if necessary after additional drying in a clean place).
Proof of the fundamental suitability of instruments for effective manual cleaning and disinfection was provided by an independent, officially accredited and recognized (Section 15 (5) German Medical Devices Act) testing laboratory using the precleaning and cleaning agent Cidezyme/Enzol and the disinfection agent Cidex OPA (Johnson & Johnson GmbH, Norderstedt). The procedure described above was taken into consideration.
Disinfection is only possible in connection with complete final sterilization of reusable cannulas. See section 6 “Sterilization”. 3. Drying Wipe any remaining water off the cannulas with a lint-free cloth. Use compressed air to remove fluids from the inner lumen of the cannula. 4. Maintenance, inspection and functional test a. Check each cannula to ensure that all visible tissue and soil has been removed.
Use an optical magnifying lens for inspection. b. Inspect the cannulas visually for damage and/or wear.
If you are in any doubt as to the correct functioning of the cannula, please contact Möller Medical GmbH. 5. Packaging Package the cannulas or sterilization trays in disposable sterilization packaging (single or double packaging) which meets the following requirements (material/process): •
DIN EN ISO/ANSI AAMI ISO 11607 (for USA: FDA clearance)
•
suitable for steam sterilization (temperature resistance up to min. 142°C (288°F) sufficient steam permeability)
•
sufficient protection of the cannulas or sterilization packaging from mechanical damage
6. Sterilization Only the sterilization methods outlined below should be used; other sterilization methods are not permitted.
page 13 to 16
Steam sterilization •
Fractionated vacuum procedure 4, 5(with sufficient product drying 6)
•
Steam sterilizer according to DIN EN 13060/DIN EN 285 or ANSI AAMI ST79 (for USA: FDA clearance)
•
Validated according to DIN EN ISO 17665 (valid IQ/OQ (commissioning) and productspecific performance qualification (PQ))
•
Maximum sterilization temperature 138°C (280°F; plus tolerance as per DIN EN ISO 17665)
•
Sterilization time (exposure time at sterilization temperature):
Country
Europe, other countries
USA
Fractionated vacuum procedure at least 4 min at 132 °C (270 °F) / 134 °C (273 °F); drying time at least 20 min at ~ 80 °C (176 °F)
at least 4 min at 132 °C (270 °F), drying time at least 20 min at ~ 80 °C (176 °F)
Gravitation procedure
not recommended
not recommended
Proof of the fundamental suitability of instruments for effective steam sterilization was provided by an independent, officially accredited and recognized (Section 15 (5) German Medical Devices Act) testing laboratory using the steam sterilizer Selectomat PL/669-2 Cl (MMM Münchner Medizin Mechanik GmbH, Planegg) and the fractionated vacuum process with 3 vacuum steps of 90 kPa, a sterilization pressure of 220 kPa and a drying pressure of ~ 90 kPa. The typical conditions in hospital and doctors’ practices and the procedure described above were taken into consideration.
The flash sterilization procedure is not permitted. Also do not use hot air sterilization, radiation sterilization, formaldehyde or ethylene oxide sterilization or plasma sterilization. 7.
Checking
Check all cannulas and their attachments after cleaning or cleaning/disinfection for corrosion, damaged surfaces, chips, soiling and discolouration. Separate out damaged cannulas (for numeric restrictions for reuse, see “Reusability”). Clean and disinfect cannulas that are still soiled again. 8. Storage Following sterilization, the cannulas must be stored dry and dust-free in the sterilization packaging.
4
at least three vacuum steps
5
The use of the less effective gravitation procedure is only permitted if the fractionated vacuum procedure is not available and requires considerably longer sterilization times as well as product-, device-, procedure- and parameter-specific validation under the sole responsibility of the user. 6
The drying time actually required depends directly on the parameters which are the sole responsibility of the user (loading configuration and density, sterilizer condition ...) and must therefore be determined by the user. Nevertheless, drying times of 20 minutes should not be undercut.
page 14 to 16
Material resistance When selecting the cleaning and disinfection agents, make sure that they do not contain the following components: •
organic, minerally and oxidizing acids (minimum pH-value allowed 5.5)
•
alkaline solution (maximum pH-value allowed 8.5, neutral/enzymatic cleaner recommended)
•
organic solvents (for example alcohol, ether, ketone, benzene)
•
oxidizing agents (for example hydrogen peroxide)
•
halogens (chlorine, iodine, bromine)
•
aromatic/halogenated hydrocarbon
Never clean the instruments with metal brushes and steel wool. Rinse aids and acidic neutralizers must never be used! The cannulas must not be exposed to temperatures in excess of 138 °C (280 °F; plus tolerance according to DIN EN ISO 17665)! Troubleshooting Problem
Possible cause
Remedy
Faulty device
Incorrect reprocessing
Contact the manufacturer
Soiling and/or residue on the cannulas after reprocessing
Incorrect reprocessing
Repeat reprocessing as per the reprocessing instructions.
Sluggish locking
Drying after reprocessing not sufficient
Extend drying time
page 15 to 16
It is the responsibility of the reprocessor to ensure that the reprocessing actually carried out with the equipment, materials and personnel used in the reprocessing facility achieves the desired results. This usually requires validation and routine monitoring of the process. If the equipment, materials and chemicals described above are not available, it is the responsibility of the reprocessor to validate his process accordingly. Observe the instructions and regulations of the relevant national legal regulations and standards.
30007064 Rev 2019-04 A
Please note that all cannulas sent to Möller Medical GmbH Service must be cleaned and sterilized before shipment.
Order number for Reprocessing instruction REF 93007064
Manufacturer: Möller Medical GmbH Wasserkuppenstraße 29-31 36043 Fulda, Germany Tel. +49 (0) 661 / 94 19 5 – 0 Fax +49 (0) 661 / 94 19 5 – 850
http://www.moeller-medical.com [email protected]
page 16 to 16